America's War on Pain Pills Is Killing Addicts and Leaving Patients in Agony
The government's efforts to get between people and the drugs they want have not prevented drug use, but they have made it more dangerous.

Craig, a middle-aged banking consultant who was on his school's lacrosse team in college and played professionally for half a dozen years after graduating, began developing back problems in his early 30s. "Degenerative disc disease runs in my family, and the constant pounding on AstroTurf probably did not help," he says. One day, he recalls, "I was lifting a railroad tie out of the ground with a pick ax, straddled it, and felt the pop. That was my first herniation."
After struggling with herniated discs and neuropathy, Craig consulted with "about 10 different surgeons" and decided to have his bottom three vertebrae fused. He continued to suffer from severe lower back pain, which he successfully treated for years with OxyContin, a timed-release version of the opioid analgesic oxycodone. He would take a 30-milligram OxyContin tablet twice a day, supplemented by immediate-release oxycodone for breakthrough pain when he needed it.

Then one day last May, Craig's pain clinic called him in for a pill count, a precaution designed to detect abuse of narcotics or diversion to nonpatients. The count was off by a week's worth of pills because Craig had just returned from a business trip and forgot that he had packed some medication in his briefcase. He tried to explain the discrepancy and offered to bring in the missing pills, to no avail. Because the pill count came up short, Craig's doctor would no longer prescribe opioids for him, and neither would any other pain specialist in town.
"I have lived my life by the rules," says Craig (whose name I've changed at his request). "I made one mistake, and they condemned me for it. They were basically saying that I'm a druggie when I have been fine for four years. My first pill count ever, and they boot me." He says a nurse at the practice told him "the doctors were getting tired of all the scrutiny, so they were booting all the opioid patients."
Without the OxyContin, Craig says, "every morning is a challenge to get out of bed." Even with liberal use of ice packs and Biofreeze, he says, "It's horrible. I can't expect to live a life like this. I'm not a junkie. I'm not a threat to society. I'm not a threat to myself. I simply want to live my life without pain."
Like other patients across the country, Craig is a victim of the recent crackdown on prescription opioids, which is based on a narrative that mistakenly blames pain treatment for a plague of addiction and death. Most Americans believe we are in the midst of an "opioid crisis" that began in the 1990s with the introduction of OxyContin. According to the generally accepted account, deceptive marketing encouraged reckless prescribing, which led to widespread addiction among patients and record numbers of opioid-related fatalities—a situation President Donald Trump has declared a public health emergency.
Former New Jersey Gov. Chris Christie, who chaired the President's Commission on Combating Drug Addiction and the Opioid Crisis, invokes that narrative when he talks about "the injured student-athlete who becomes addicted after [his] first prescription" or remembers the law school classmate who died of an overdose after getting hooked on the oxycodone he was taking for back pain. Such examples are misleading because they are rare, accounting for only a small percentage of opioid-related deaths.
Contrary to the impression left by most press coverage of the issue, opioid-related deaths do not usually involve drug-naive patients who accidentally get hooked while being treated for pain. Instead, they usually involve people with histories of substance abuse and psychological problems who use multiple drugs, not just opioids.
Conflating those two groups results in policies like the pill count that left Craig without the pain medication he needed to get out of bed in the morning, go to work, and lead a normal life. The rationale is that cutting people like him off will stop them from ending up dead of an overdose in a Walmart parking lot next to a baggie of fentanyl-laced heroin.
But the truth is that patients who take opioids for pain rarely become addicted. A 2018 study found that just 1 percent of people who took prescription pain medication following surgery showed signs of "opioid misuse," a broader category than addiction. Even when patients take opioids for chronic pain, only a small minority of them become addicted. The risk of fatal poisoning is even lower—on the order of two-hundredths of a percent annually, judging from a 2015 study.
Despite such reassuring numbers, the government is responding to the "opioid epidemic" as if opioid addiction were a disease caused by exposure to opioids, a simplistic view that ignores the personal, social, and economic factors that make these drugs attractive to some people. Treating pain medication as a disease vector, the government has restricted access to it by monitoring prescriptions, investigating doctors, and imposing new limits on how much can be prescribed, for how long, and under what circumstances. That approach hurts pain patients by depriving them of the analgesics they need to make their lives livable, and it hurts nonmedical users by driving them into a black market where the drugs are deadlier.
A large majority of opioid-related deaths now involve illicitly produced substances, primarily heroin and fentanyl. As usual, the government's efforts to get between people and the drugs they want have not prevented drug use, but they have made it more dangerous.
'Highly Addictive Drugs'
"We've known for millennia that opioids are highly addictive drugs," says Andrew Kolodny, executive director of Physicians for Responsible Opioid Prescribing. "We have an epidemic of people with the disease of opioid addiction in the United States. The reason it's become an epidemic is because opioids have been overprescribed by my colleagues, who were led to believe that we didn't have to worry about addiction."
Kolodny, who is also co-director of opioid policy research at Brandeis University's Heller School for Social Policy and Management, says the American Pain Society and the American Academy of Pain Medicine (AAPM) started to "advocate for opioids" in the late 1990s, taking the position that "the risk of addiction has been overblown, even that the risk of overdose death has been overblown, and that we should be prescribing much more for people with chronic pain." As a result, he says, "we got our patients addicted, and we stocked people's medicine chests with addiction, so their kids wound up getting addicted."
This gloss is superficially plausible. According to the U.S. Centers for Disease Control and Prevention (CDC), the amount of opioids prescribed in the United States more than quadrupled between 1999 and 2010, rising from 180 to 782 morphine milligram equivalents (MME) per capita. During the same period, according to CDC data, the annual number of deaths involving the kinds of opioids prescribed for pain also roughly quadrupled, from about 4,300 to about 18,500.
The relationship is not quite as straightforward as it might seem. Opioid prescriptions, measured by MME per capita, fell by nearly a fifth from 2010 to 2015, while deaths involving these drugs continued to rise. The CDC's numbers also indicate that deaths involving opioid pharmaceuticals are not always more common in states with higher prescription rates. In 2015, for instance, West Virginia's death rate was more than twice as high as Tennessee's, although it had fewer opioid prescriptions per capita. Rhode Island, New Mexico, and Utah had higher death rates than Oklahoma, where opioids were prescribed substantially more often.
Still, the expansion of the legal market for opioids obviously had something to do with the increase in illegal use of these drugs. Many of the pills were diverted to nonmedical users, either after they were prescribed or through theft from points higher in the distribution chain.
But greater availability of prescription opioids cannot by itself explain the rise in addiction and drug-related deaths. "The question is why so many communities were so vulnerable to developing problems with opioids in the first place," says Daniel Raymond, policy director at the Harm Reduction Coalition. Part of the answer, he thinks, can be found in the same factors that helped elect Donald Trump. "These pockets of the Rust Belt and Appalachia, with the loss of manufacturing jobs or traditional industry jobs, were extremely primed for developing a drug problem," he says. "It happened to be opioids, but it could have just as easily been—and arguably it has also been—alcohol or methamphetamine."
When Kolodny says "we got our patients addicted," he discounts the way unhappy circumstances, such as unemployment and dim economic prospects, make drug use more appealing. He also implies that pain treatment has been the main route to opioid addiction during the last two decades. But that is not what the evidence indicates.
According to a 2014 analysis of data from the National Survey on Drug Use and Health (NSDUH), 54 percent of nonmedical users got prescription opioids for free from friends or relatives. Another 16 percent bought or stole pills from friends or relatives, while 4 percent bought them from strangers. About 6 percent mentioned other sources, including online purchases, forged prescriptions, and theft from doctors' offices or pharmacies. Just 20 percent of nonmedical users said they obtained opioids through prescriptions written for them.
Although some people who now obtain opioids indirectly may have had prescriptions at some point, these results undercut the notion that nonmedical users typically start as bona fide patients. Even among the heaviest users, just 27 percent had prescriptions at the time of the survey, and it is not clear how many of those were legitimate at the outset. In most cases, says Sidney Schnoll, a physician specializing in addiction and pain treatment who works for the consulting firm Pinney Associates, "These are people who were drug-seeking. They are not people who went to a physician, got a prescription, and suddenly became addicted to the drug."
Stefan Kertesz, a University of Alabama at Birmingham internist who, like Schnoll, specializes in pain and addiction, agrees that the prevalence of iatrogenic opioid addiction (that is, addiction resulting from medical treatment) has been exaggerated. "I think a meaningful percentage did start in care of pain," he says, "but everything I've read leaves me with the sense that the overwhelming majority of the people who are dying of overdose began with diverted pills."
The NSDUH data reinforce the impression that doctors frequently prescribe more pain pills than their patients end up needing. People who take opioids after an injury or surgery might receive enough pills for two weeks but use only half of them. It seems likely that diverted opioids more often come from such short-term prescriptions than from medication prescribed for people suffering from severe chronic pain, who probably are not keen to share or sell the drugs that keep their agony at bay.
The fact that people frequently have leftover opioids that they give away, sell, or leave in their medicine cabinets to be swiped suggests these drugs are not quite as irresistible as they are reputed to be. According to NSDUH, 98 million Americans used prescription analgesics in 2015, legally and illegally. Judging from their responses to survey questions, about 2 million of them—slightly more than 2 percent—qualified for a diagnosis of "substance use disorder" (SUD) at some point during the previous year.
SUD is a catchall category that subsumes what used to be known as "substance abuse" and the more severe "substance dependence." The Substance Abuse and Mental Health Services Administration, which oversees NSDUH, does not report the breakdown between mild, moderate, and severe SUDs. But based on this survey, it looks like somewhere between 1 percent and 2 percent of prescription opioid users experience addiction in a given year. By comparison, NSDUH data indicate that 9 percent of past-year drinkers had an alcohol use disorder in 2015. That group was about evenly divided between "abuse" and "dependence."
'Narcotics Are Not That Appealing'
Stanton Peele, a psychologist and addiction expert, observes that, contrary to conventional wisdom, "narcotics are not that appealing" to most people. In addition to the NSDUH data, he cites research finding that hospital patients who are allowed to self-administer pain medication tend to take less than those who get it on a fixed schedule. "On their own," he says, "people only use it when they're in pain."
The notion that opioid addiction is "an equal-opportunity destroyer," as politicians and drug treatment boosters like to say—or that "everyone is at risk and every family prey to loss," as Mitchell Rosenthal, founder of the Phoenix House treatment centers, told the Christie commission—is "absolutely false," Peele says. To the contrary, opioid addiction is strongly associated with unemployment, poverty, family dysfunction, and pre-existing psychological issues. Well-adjusted people with supportive families, strong social ties, and good economic prospects are much less likely to seek refuge in opioids than people who lack those advantages. To put it another way, mere exposure to opioids does not produce addiction. A drug will become the focus of a tenacious habit only if it serves an important function in the user's life.
"I didn't realize how much I was trying to run away from myself," says Jill, a former heroin user from Ohio who has been anxious since childhood, received a diagnosis of obsessive compulsive disorder as an adult, and was a victim of sexual assault in college. "I wasn't really cognizant of how difficult it was to be in my own head. I'd had a lot of trauma that I wasn't dealing with, and everything was piling up. The appeal of heroin was it turned everything off. It was like a vacation." In rehab, Jill realized that other opioid users had similar issues. "They either have a trauma or a mental illness that they're trying to deal with," she says, "and nobody gave them the tools to do that."
Kolodny concedes that most people who use opioids do not develop an addiction. "You don't become addicted by using a highly addictive drug once or twice," he says. "You can use a highly addictive drug on an intermittent basis and not get addicted. It's repeated use that puts people at very high risk of becoming addicted."
But even in studies of patients who take pain medication repeatedly and regularly, sometimes for months or years, the addiction rates are generally modest. As Nora Volkow, director of the National Institute on Drug Abuse, and A. Thomas McLellan, a former deputy director of the Office of National Drug Control Policy, noted in a 2016 New England Journal of Medicine article, "Addiction occurs in only a small percentage of persons who are exposed to opioids—even among those with preexisting vulnerabilities."
A 2010 analysis in the Cochrane Database of Systematic Reviews found that less than 1 percent of patients taking opioids for chronic pain experienced addiction. A 2012 review in the journal Addiction likewise concluded that "opioid analgesics for chronic pain conditions are not associated with a major risk for developing dependence."
A study reported in The BMJ this year tracked 568,612 opioid-naive patients who took prescription pain medication following surgery and found that 5,906, or 1 percent, showed signs of "opioid misuse" during the course of the study, which included data from 2008 through 2016. Although some studies have described "rates of misuse, abuse, and addiction-related aberrant behaviors" as high as 26 percent among chronic pain patients, Volkow and McLellan reported, "rates of carefully diagnosed addiction" average less than 8 percent.
Fatal overdoses among patients are even rarer. A 2015 study reported in the journal PLOS One followed chronic pain patients treated with narcotics for up to 13 years and found that one in 550 died from an opioid-related overdose, which is a risk of less than 0.2 percent over the course of the study. A 2015 study of opioid-related deaths in North Carolina, reported in Pain Medicine, found 478 fatalities among 2.2 million residents who were prescribed opioids in 2010, an annual rate of 0.022 percent.
Kolodny cites a 2012 study of deaths involving prescription opioids in Utah, reported in the Journal of General Internal Medicine, to support his contention that iatrogenic addiction accounts for "the bulk of the overdose deaths." In 87 percent of the cases, relatives or other people who knew the decedents said they had received prescriptions for pain medication in the previous year.
Other studies, however, indicate that prescribed drugs play a smaller role in opioid-related fatalities than that number suggests. In the North Carolina study, only half of the decedents had active prescriptions for opioids when they died. A 2008 study of West Virginia deaths involving opioid analgesics, reported in the American Medical Association journal JAMA, found that most of the decedents had never been prescribed opioids. A 2012 study of opioid users in Maine, reported in Addictive Behaviors, found that two-fifths reported chronic pain, but more than three-quarters of those subjects said their opioid use preceded their symptoms. A 2014 study of people who were treated in emergency rooms for overdoses involving prescription opioids, reported in JAMA Internal Medicine, found that just 13 percent had a chronic pain diagnosis.
Even when someone who dies from drug poisoning has an opioid prescription, it does not necessarily mean he was a bona fide patient. Patients can fool doctors, and some doctors are eager to be fooled. "Pill mill" cases in Florida and West Virginia have involved doctors who saw as many as 70 patients a day, each of whom paid $100 to $300 in cash, and doctors who wrote prescriptions without meeting patients or looking at their files. Such examples do not tell us much, if anything, about legitimate patients who become addicted while being treated for pain.
"These pockets of the Rust Belt and Appalachia, with the loss of…traditional industry jobs, were extremely primed for developing a drug problem."
Whatever share of people who die from drug poisoning began using opioids as legitimate patients, the share of patients taking opioids who die from drug poisoning is tiny—and the risk is not random. In the Utah study cited by Kolodny, 61 percent of the decedents had used illegal drugs, 80 percent had been hospitalized for substance abuse (including abuse of alcohol and illegal drugs as well as prescription medications), 56 percent had a history of mental illness, and 45 percent had been hospitalized for psychiatric reasons other than substance abuse.
NSDUH data indicate that most nonmedical users of prescription opioids use other drugs as well, a fact that is reflected in mortality data. In the West Virginia study, 79 percent of the deaths involved combinations of drugs. In North Carolina, benzodiazepines such as Valium and Xanax were detected in 61 percent of the people whose deaths were attributed to prescription opioids, and that's just one class of depressants. In New York City, which has one of the country's most thorough systems for recording causes of death, 97 percent of drug-related deaths involve more than one substance. A 2003 study of 919 deaths attributed to oxycodone, reported in the Journal of Analytical Toxicology, likewise found that 97 percent involved combinations of drugs.
It seems clear that people by and large are not dying simply by taking too many pain pills. Even Chris Christie's law-school friend washed down his Percocet with vodka.
What's true of prescription analgesics is also true of illegal opioids. So-called overdose deaths generally involve mixtures of drugs, as reflected in the toxicology results for celebrities such as John Belushi (heroin and cocaine), River Phoenix (heroin, cocaine, and diazepam), Chris Farley (heroin and cocaine), Cory Monteith (heroin and alcohol), and Philip Seymour Hoffman (heroin, cocaine, amphetamines, and benzodiazepines). It is misleading to call such deaths "overdoses" (as opposed to, say, "mixed drug intoxication," the phrase used by the medical examiner who handled Hoffman's case), since people who die after taking an opioid along with other substances might still be alive if they had taken the opioid by itself.
Heroin Gets Deadlier
As these examples suggest, attributing deaths to particular drugs can be tricky, especially since methods for making that determination vary widely from one jurisdiction to another. But one thing is clear: Prescription analgesics are no longer the main factor in opioid-related deaths. In 2013 and 2014, according to an analysis by the Massachusetts Department of Public Health, 85 percent of opioid-related fatalities in that state involved heroin and/or fentanyl. A prescription analgesic was the deadliest drug in just 5 percent of the cases.
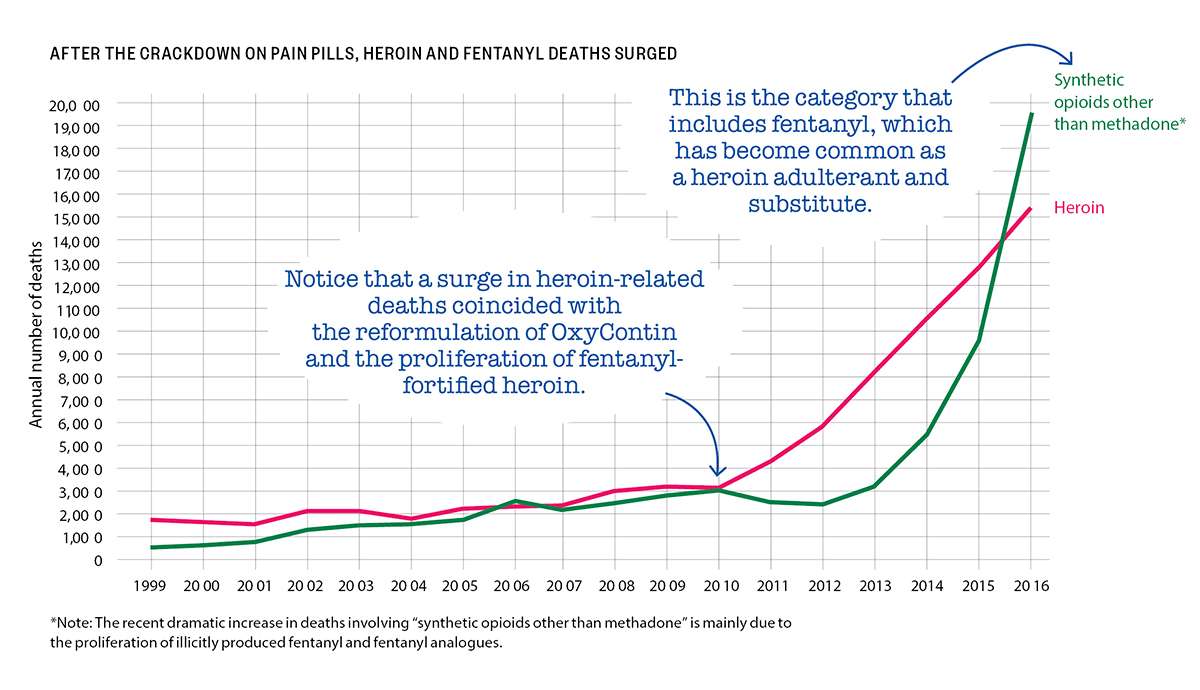
National data show a similar pattern. The CDC says there were more than 42,000 opioid-related deaths in 2016, including about 15,500 deaths involving heroin. About 19,400 deaths involved "synthetic opioids other than methadone," a category that consists mainly of fentanyl and its analogues, which nowadays are generally manufactured by drug traffickers rather than pharmaceutical companies. Prescription analgesics were implicated in about 17,900 drug poisoning fatalities.
Since some deaths involve more than one opioid, the total is smaller than the sum of the subcategories. But the CDC's numbers indicate that just two-fifths of opioid-related deaths in 2016 involved prescription analgesics, and some of those deaths also involved heroin, fentanyl, or its analogues.
Fentanyl is roughly 40 times as potent as heroin, which helps explain its appeal to drug dealers, who can use it to smuggle more doses in the same volume and to boost the impact of heroin that has been diluted by cutting agents. The increased use of fentanyl makes the potency of black-market heroin, which was always unpredictable, even more variable, raising the risk of fatal drug poisoning.
Indeed, heroin-related deaths, which began rising gradually in 2005, quintupled between 2010 and 2016. Deaths involving the category of opioids that includes fentanyl more than tripled between 2010 and 2015, then doubled in 2016 alone.
During the same period when heroin-related deaths rose by 400 percent, the number of heroin users counted by NSDUH rose by just 53 percent. NSDUH probably misses a lot of heroin users, both because respondents are especially reluctant to admit using that drug and because the survey sample does not include people who are institutionalized or have no fixed residence. But the NSDUH data still should give us a pretty good sense of how much the group of heroin users has expanded, if not its absolute size. And those data indicate that the number of heroin deaths has increased roughly eight times as fast as the number of heroin users.
To put it another way, heroin was eight times deadlier in 2016 than it was in 2010. The proliferation of fentanyl-fortified heroin is the most obvious explanation.
A research team headed by Brown University medical anthropologist Jennifer Carroll found that fear of fentanyl was common among the Rhode Island opioid users they interviewed for a study reported in The International Journal of Drug Policy last year. "Participants who were aware of fentanyl universally described it as dangerous and potentially deadly," Carroll and her colleagues write. "People are dropping like flies," one heroin user said. "I don't want to die," said another, explaining why he buys heroin only from a dealer he trusts not to sell him fentanyl-laced powder. Others said they try to avoid fentanyl and take "test hits"—small trial doses—whenever they suspect it is present.
Many of the people who are dealing with black-market powders of unknown composition were previously accustomed to the predictable doses of legally manufactured analgesics. "I used to take just the pills, and then I started doing dope, the heroin, only when I could get it, when it was cheaper," said a female opioid user quoted by Carroll and her collaborators. "But I don't prefer it because you never know what you're getting. It's scary, so I'm more into pills."
She was right to be scared. Comparing deaths counted by the CDC to users counted by NSDUH indicates that heroin is more than 10 times as lethal as prescription opioids. Even if that calculation exaggerates the difference because NSDUH undercounts heroin users, it seems clear that switching from prescription opioids to black-market substitutes dramatically increases the risks that users face.
Despite the dangers, that sort of switch is much more common today than it used to be. A 2014 study of heroin users entering treatment, reported in JAMA Psychiatry, found that 80 percent of those who began using opioids in the 1960s started with heroin. By contrast, Washington University neuropharmacologist Theodore Cicero and three other researchers noted, 75 percent of those whose opioid abuse began in the 2000s "reported that their first regular opioid was a prescription drug." (That does not necessarily mean it was prescribed for them.)
A more recent study led by Cicero, reported last year in the journal Addictive Behaviors, suggests that trend has reversed. Cicero and his co-authors report that a 2015 survey of people entering treatment for opioid use disorder found 33 percent had started with heroin, up from 9 percent in 2005. That finding is consistent with the hypothesis that troubled people who find emotional relief in drugs will turn to whatever options are most readily available. During the period when Cicero found that more and more opioid users were starting with heroin, pain pills were becoming harder to obtain thanks to surveillance, tighter regulations, and investigations of doctors.
"As the most commonly prescribed opioids—hydrocodone and oxycodone—became less accessible due to supply-side interventions, the use of heroin as an initiating opioid has grown at an alarming rate," Cicero and his co-authors conclude. "Given that opioid novices have limited tolerance to opioids," they add, the variability in potency typical of the black market poses a special risk to them, which is "likely to be an important factor contributing to the growth in heroin-related overdose fatalities in recent years."
'You Have to Start Somewhere'
To the extent that the crackdown on prescription analgesics has made them more expensive and harder to get, it has pushed opioid users toward more dangerous drugs. That helps explain why total opioid-related fatalities more than tripled from 2002 to 2016, even as illegal use of pain pills declined.
"We're funneling them from those drugs that were FDA-approved, you know what the dose was, they were predictable, towards drugs that are less predictable and more likely to cause overdose," says Daniel Raymond, whose work at the Harm Reduction Coalition involves finding ways to make drug use less lethal. With legally produced opioids, he says, "I have this zone that I stay in, and that's anchored by the fact that I know exactly what dose is in each pill. If I'm buying heroin every day…I never know the relative potency and concentration that I'm getting. I might be going to different dealers, and one week there's fentanyl in my heroin, and the next week there's not. I cannot self-titrate. I cannot optimize my dosing to stay within that window where I'm not going through withdrawal but I'm not at risk of overdose."
In a 2017 interview with the Carlisle Sentinel, Carrie DeLone, Pennsylvania's former physician general, confessed that "we knew that this was going to be an issue, that we were going to push addicts in a direction that was going to be more deadly." Her justification: "You have to start somewhere."
For a sense of where that attitude can lead, consider what happened after the reformulation of OxyContin. Introduced in 1996, the drug was widely blamed for the subsequent rise in opioid-related deaths, even though most of those deaths actually involved short-acting pain pills.
In 2007, Purdue Pharma, the company that makes OxyContin, pleaded guilty to "misbranding" the product by minimizing its abuse potential. Three years later, the Food and Drug Administration approved a new, "abuse-deterrent" formulation of the drug, which was designed to make it harder to crush and snort or inject. When the reformulated OxyContin is mixed with water, it forms a gel.
The old version of OxyContin was withdrawn from the market when the new one was introduced, a switch that coincided with the post-2010 spike in heroin-related deaths. In a 2017 paper published by the National Bureau of Economic Research, Wharton School health economist Abby Alpert and two RAND Corp. researchers investigate whether those developments were related by comparing states with different pre-2010 rates of nonmedical OxyContin use.
"We estimate large differential increases in heroin deaths immediately after reformulation in states with the highest initial rates of OxyContin misuse," Alpert and her colleagues write. "Our results imply that a substantial share of the dramatic increase in heroin deaths since 2010"—perhaps as much as 80 percent—"can be attributed to the reformulation of OxyContin." They conclude that the increase in heroin-related fatalities offset any decrease in OxyContin-related fatalities, "leading to no net reduction in overall overdose deaths."
There is some evidence that prescription drug monitoring programs, which allow regulators and law enforcement agencies to track the controlled substances a doctor prescribes, also have led people to substitute illicitly produced drugs for pills. A 2017 study reported in The American Journal of Managed Care found that such programs, which by 2015 had been adopted by every state except Missouri, "were not associated with reductions in drug overdose mortality rates and may be related to increased mortality from illicit drugs and other, unspecified drugs."
Harm Maximization
Responding to the shift from prescription analgesics to heroin and fentanyl, drug warriors have further magnified the dangers opioid users face by cracking down on those markets. A heroin user who tries to avoid fentanyl by sticking with a dealer he deems trustworthy may face increased risks if that dealer is arrested. Similarly, the FBI may be endangering drug users when it shuts down websites that help reduce hazards to consumers by selling fentanyl-free heroin or offering opioids in uniform liquids that make dosing easier.
Arresting opioid users also increases the risk of a fatal drug reaction, since abstinence imposed by jail or mandatory treatment reduces their tolerance. Once they get out, the doses to which they were accustomed before they were arrested may prove lethal. "There's one study that shows that someone's risk of overdose in the two weeks following their release from incarceration is up to 25 times higher than it is normally," says Carroll, the Brown University medical anthropologist. "People are overdosing right after they get out of prison."
Another policy that almost seems designed to make fatal poisoning more common is charging people with homicide if someone dies after taking a drug they supplied. Because prompt medical attention is crucial in saving people from potentially lethal opioid reactions, 40 states and the District Columbia have enacted "911 Good Samaritan" laws that shield bystanders from certain drug-related charges when they call for help. But if those bystanders know they might be prosecuted for murder should rescue attempts fail, they will think twice before dialing 911.
According to a 2017 report from the Drug Policy Alliance (DPA), 20 states have laws that specifically address drug-induced homicide, while others "charge the offense of drug delivery resulting in death under various felony-murder, depraved heart, or involuntary or voluntary manslaughter laws." Potential prison sentences range from two years to life, which is the minimum penalty in six states; the death penalty is possible in Colorado and Florida. Under federal law, drug distribution resulting in death or serious injury is punishable by 20 years to life. These statutes have been on the books since the 1980s, but prosecutions seem to have risen sharply in recent years, judging from mentions in news stories, which by the DPA's count more than tripled between 2011 and 2016, from 363 to 1,178 per year.
Although politicians may claim that drug-induced homicide prosecutions are aimed at high-level dealers, the targets are usually people close to the decedents. Someone's role in "distributing" the drug may be limited to buying it for someone else or sharing a stash. Even when money changes hands, the dealers are often selling just enough to finance their own habits. Cases cited by the DPA include a small-time New Hampshire dealer who did not realize the heroin he sold a friend contained fentanyl but got 10 to 30 years anyway, an Ohio woman who got three years after she took heroin with her father and woke up to find him dead, and a Minnesota woman who got six years because her husband died after taking methadone prescribed for her, even though she called 911 and tried to save his life.
"The vast majority of charges," the DPA says, "are sought against those in the best positions to seek medical assistance for overdose victims—family, friends, acquaintances, and people who sell small amounts of drugs, often to support their own drug dependence." The report concludes that "the only behavior that is deterred by drug-induced homicide prosecutions is the seeking of life-saving medical assistance."
One widely endorsed policy that actually holds promise for reducing drug-related deaths is easier access to naloxone, a.k.a. Narcan, an overdose-reversing opioid antagonist that can be administered by injection or nasal spray. Dispensing naloxone along with pain medications, making it available without a prescription (which 41 states currently allow), supplying it to first responders, and distributing it to friends and relatives of opioid users are ways to increase the odds that it will be used promptly when someone needs it. Speed is especially important when a person overdoses on fentanyl, which can cause lethal respiratory depression faster than heroin.
"I have a four-milligram Narcan in my purse right now," says Jill, the former heroin user in Ohio, who adds that she has "Narcanned" friends "probably dozens" of times. "You hope you don't have to use it, but you might have to. Everyone should have one. That is the only way that I can see the epidemic being managed at all."
For some drug warriors, naloxone's lifesaving potential is a bug, not a feature. In 2016 Maine Gov. Paul LePage, a Republican, vetoed a bill allowing pharmacists to dispense naloxone without a prescription. "Naloxone does not truly save lives; it merely extends them until the next overdose," he wrote in his veto letter. "Creating a situation where an addict has a heroin needle in one hand and a shot of naloxone in the other produces a sense of normalcy and security around heroin use that serves only to perpetuate the cycle of addiction."
LePage's argument is familiar from the debate over needle exchange programs: For the sake of deterrence, he thinks, drug use should be as dangerous as possible. Maine legislators, who overrode LePage's veto, apparently disagreed.
How to Not Die
Drug testing is another promising form of self-help. Test strips and reagent kits that cost a dollar or two each can tell opioid users if the powder they just bought contains fentanyl. Some tests also detect common fentanyl analogues. A recent pilot study in Vancouver found that 83 percent of drugs thought to be heroin tested positive for fentanyl. Drug users were 10 times as likely to take less than usual and 25 percent less likely to overdose if they tested their drugs before injecting.
"It becomes this concrete, physical manifestation that opens up a conversation about fentanyl risks," the Harm Reduction Coalition's Raymond says. "If we've got fentanyl in our community, whatever you've been doing to minimize or avoid overdose, you need to up your game because it might not be enough against fentanyl. If you're careful about how much you use, if you're careful about what dealers you buy from, you might need to start thinking about not using alone and making sure you've got extra naloxone on hand."
The fact that drug mixtures figure in the vast majority of deaths involving heroin and other opioids suggests that discouraging particularly dangerous combinations could save lives—assuming it actually has an impact on people's behavior. "I think there's a huge role for education around that," Carroll says, citing a spate of heroin-related deaths in the late 1990s among high school students in Plano, Texas, some of whom died after snorting the drug while drinking. "It was just a pure educational gap, because I don't think there was any reason to believe that anyone was being deliberately cavalier. Educating people about how to not die is always worth our time."
Jill, the former heroin user, is less sanguine. "You're telling somebody, 'Don't mix benzos with heroin because it potentiates the heroin,'" she says. "They will mix the benzos with the heroin because they want to potentiate the heroin. One of the earliest things I learned was that if you take benzos it'll make your high better."
Raymond agrees that people who like to mix drugs and have done it repeatedly without any close calls won't be very receptive to the message that they are being reckless. "What we want to address is the environment of risk," he says. "And we can do that by saying, 'Hey, make sure that you have naloxone available. Don't use alone.' We can do that by talking about things like supervised injection facilities."
Such facilities provide a safe environment where people can take drugs they bring with them under medical supervision and get help immediately if they need it. The facilities may also offer services such as drug testing, syringe exchange, and assistance finding treatment. Studies of Insite, a supervised injection facility that has been operating since 2003 in Vancouver, have found that it boosted treatment admissions and reduced public drug use, needle sharing, and opioid-related deaths without raising local crime rates.
As a risk reduction strategy, letting people inject drugs at a place like Insite represents a distinct improvement over having them do it in the restroom at the public library in the hope that if they overdose they'll be discovered before it's too late. The first government-sanctioned supervised injection facilities in the United States are expected to open this summer in San Francisco. Officials in Seattle and Philadelphia are also interested in the idea.
Raymond notes that naloxone and needle exchanges "have gained increasing acceptability and, to varying degrees, lost their aura of controversy." But now that policy makers are beginning to talk about allowing supervised injection facilities, he says, "it's almost like a flashback to the '90s," when opponents of syringe exchanges argued that they should not be allowed because they encourage drug use. "It forces people to confront the question of how we feel about people using drugs and what are we willing to do to save their lives," he says. "The fact that it's even on the table is a testament to how far we've come."
People by and large are not dying simply by taking too many pain pills. Even Chris Christie's classmate washed down his Percocet with vodka.
So-called medication-assisted treatment, which combines counseling and behavioral therapy with substitute opioids, is not as controversial as supervised injection facilities. Research indicates that methadone, which has been used as a treatment for heroin addiction since the 1960s, reduces treatment dropout rates, heroin use, drug-related fatalities, and criminal activity. Buprenorphine seems to be about as effective as methadone at keeping users in treatment, reducing heroin use, and preventing premature death. Methadone is very strictly regulated, available only at special clinics that enrollees must visit to consume their daily doses. Buprenorphine is more widely available, but caps on the number of people a doctor can treat and conditions for prescribing it, including at least eight hours of special training and a federal waiver, make it harder to get than it should be.
Methadone and buprenorphine are the only opioids that can legally be prescribed for addiction treatment or maintenance in the United States. A wider range of options, including analgesics such as hydromorphone (a.k.a. Dilaudid) or diacetylmorphine (a.k.a. pharmaceutical heroin), probably would make treatment more attractive and therefore more effective for a wider range of people. Heroin is banned for all uses in the United States, but heroin maintenance is legal in Belgium, Canada, Denmark, Germany, Great Britain, the Netherlands, and Switzerland. Studies show it is more effective than methadone at promoting retention, reducing illicit drug use, and improving health outcomes.
Heroin maintenance "can be effective for people who have not had success with something like methadone," Raymond says. Even for people who eventually end up on methadone, "it may be an intermediate step to transition people off of a street supply of heroin." That switch alone would improve the odds of survival, since the potency of legally produced opioids is consistent and predictable.
"It's not clear at all, when we review the data, that there's a painkiller epidemic or a heroin addiction epidemic," Peele, the psychologist, says. "There's a death epidemic, and the way to address that is to guarantee the best, most regular, and purest supplies of drugs." Schnoll, the pain and addiction specialist, agrees that "if people can get their drug at a reasonable cost, knowing the purity of it, being able to use it safely, people are going to migrate to that."
Punishing Patients
In contrast with these harm reduction tactics, continuing attempts to discourage the use of prescription pain medication promise to cause a lot of needless suffering without making a noticeable dent in opioid-related deaths. Prescription guidelines that the CDC issued in March 2016, which minimize the benefits of opioids, exaggerate their risks, and encourage doctors to be stingy with them, exemplify this misguided strategy.
A 2016 critique published by the journal Pain Practice challenges several key aspects of the CDC document, including its recommended dose ceilings, its general declaration that nonopioid treatment is "preferred for chronic pain," its suggestion that opioid prescriptions for acute pain last no longer than seven days, and its statement that doctors who decide to prescribe opioids should begin with immediate-release products rather than extended-release or long-acting (ER/LA) analgesics.
The criticism of that last recommendation sums up what is wrong with the guidelines in general. "It appears that this statement is asking physicians to make prescribing choices based on public health concerns…rather than the most appropriate course of therapy for the individual patient," write pain specialist Joseph Pergolizzi and the six other authors of the Pain Practice article. "If prescribers must forego the use of ER/LA opioids in patients who could possibly benefit from them, it essentially punishes the chronic pain patient for offenses committed by drug abusers."
The CDC guidelines in themselves are not legally binding. But Congress has imposed them on the Department of Veterans Affairs (V.A.), and at least 18 states have enacted elements of them. In 2016 and 2017, according to a tally by the National Conference of State Legislatures, 14 states imposed limits on the duration of initial prescriptions for acute pain, ranging from three days (Kentucky) to two weeks (Nevada), with seven days the most common. Arizona enacted a similar law in January. Four states (Arizona, Maine, Nevada, and Rhode Island) have imposed daily dose ceilings, while Maryland limited opioid prescriptions to "the lowest effective dose" and a quantity "not greater than needed for the expected duration of pain." The legislatures of seven other states directed or authorized other bodies to impose limits on opioid prescriptions.

In addition to these statutory changes, the CDC guidelines are shaping the policies and practices of regulators, insurers, and law enforcement agencies. Doctors face "pressure from many directions," the University of Alabama at Birmingham's Kertesz notes. That includes "scrutiny from state officials," "barriers from insurance and pharmacy benefit plans," "more restrictive guidelines from state licensing boards," "stories of some physicians losing their livelihoods and being shut down," and "super-intense rhetoric from thought leaders and journalists," who tend to blame physicians for causing the "opioid epidemic" through careless prescribing. "Under that kind of pressure," Kertesz says, "who wouldn't change what they're doing, even if it hurts a few patients?"
Some physicians have decided the safest course is to stop prescribing opioids altogether. "There are many pain clinics flooded with patients who have been treated previously by their primary care physician," says Jianguo Cheng, president-elect of the AAPM. These refugees include patients who "have been functional" and "responding well" to opioids for "many years."
Schnoll sees similar problems. "Pain is still undertreated, and unfortunately it's getting worse because of the backlash that's occurring," he says. "I still get calls from patients whom I treated years ago, who were on stable doses of medication, doing very well, who have chronic pain conditions, and they can't get medication to treat their pain. They're being taken off medication on which they had done very well for years."
One such patient, a former cable company salesman named John, successfully used OxyContin to treat the back pain caused by injuries sustained during a mugging in 2011. Before he found a medication that worked for him, he recalls, "my wife was about to leave me, because I was a miserable bastard. When you're in that much pain, you want to just go to sleep and not wake up."
After the CDC guidelines came out, John was told that his daily dosage had to be cut in half. "My whole life turned upside down in a matter of 30 days," he says. "I'm back in bed now. I can't really get up very much, and I'm right back where I started in 2011."
'Can't Take It Anymore'
Maxx Lamb, a Kansas college student, became a pain treatment activist as a result of his experience with Ehlers-Danlos syndrome, a hereditary connective tissue disorder. He sent me a photograph of a sign at a doctor's office in Washington state that reflects the impact of the CDC's guidelines. "Beginning February 2017," it says, "Morphine Equivalency Dosing WILL decrease until CDC guidelines are met by June 2017. Target is 90mg of Morphine equivalency per day, or less. All medication adjustments will be based on this new clinic policy."
The CDC guidelines do not explicitly say patients should never exceed 90 morphine milligram equivalents a day, but they do suggest that such doses are hard to defend. "Clinicians should use caution when prescribing opioids at any dosage," the CDC says, and "should carefully reassess evidence of individual benefits and risks when considering increasing dosage" to 50 MME per day or more. The guidance adds that doctors "should avoid increasing dosage" above 90 MME per day, or at least "carefully justify a decision to titrate dosage" above that level.
Although the CDC implies there is something special about these numbers, the study of opioid-related deaths in North Carolina found that "dose-dependent opioid overdose risk among patients increased gradually and did not show evidence of a distinct risk threshold." Critics see the CDC's cutoffs as arbitrary, since patients vary widely in the way they metabolize and respond to opioids, especially if they have developed tolerance after years of treatment.
"There seems to be no clear clinical evidence that opioid risks increase with 50 MME/day or that doses should never exceed 90 MME/day in any patient," Pergolizzi et al. write. "It seems unnecessary and counterproductive to decrease a patient's dose of opioids just to achieve an arbitrary limit."
CDC officials say they do not want doctors to impose dose reductions on patients. "We do hear stories about people being involuntarily taken off opioids," Deborah Dowell, a co-author of the guidelines, said at an April 2017 conference. "We specifically advise against that in the guidelines."
That's not exactly true, but the guidelines do describe tapering as a consensual process. The CDC says "clinicians should work with patients to reduce opioid dosage or to discontinue opioids" if they determine that the risks outweigh the benefits. It notes that "tapering opioids can be especially challenging after years on high dosages" but says "these patients should be offered the opportunity to re-evaluate their continued use of opioids at high dosages."
In many cases, that "opportunity" has become a unilateral decision. "Even though it is not specified in the CDC guidelines to do this," Kertesz says, "I am seeing many physicians in my region and across the country taper patients against their will. They're tapering stable patients who were not violating the rules of the practice, who were basically functional. Physicians are tapering them without consent, often in a draconian fashion, and in many cases simply discharging the patient from the practice and just ending the clinical relationship."
Lynn Webster, a pain researcher and former AAPM president, says he gets emails almost every day from desperate patients. Many had been taking doses of opioids that controlled their pain well enough for them to work and "have a reasonable life…maybe for a decade or more." Now, "because they're being forced to take a dose far less than what has been necessary to keep them functional," they are bedridden.
Other patients "have been told by their doctors that they're taking them off all of their medicines," Webster says. Many of them "don't have any idea where to go to get help." Some say "the only option they have is suicide."
Kertesz quotes a doctor at "a large integrated care system" who reported that "the situation of chaotic and involuntary tapers was brought home to me by a patient who shot himself in our parking lot." That patient survived. Others have not.
Lamb, the pain treatment activist, has compiled a list of two dozen patients who have committed suicide in the last few years after they were denied adequate pain treatment. They include Allison Kimberly, a 30-year-old Colorado woman with interstitial cystitis, who killed herself in June 2017 after an emergency room turned her away.
"I was rushed to the ER because my pain was so out of control I couldn't take it anymore," Kimberly wrote on Instagram. "I got ZERO help. After 7 hours I was discharged. The nurse has the nerve to say that my kind of pain shouldn't be that bad and basically I was faking for medication. I am so beside myself I am shaking as I type this. Screaming and begging in pain, needing any kind of help they'd give me and I was just sent home."
Kevin Keller, a 52-year-old Navy veteran with severe pain following a stroke, shot himself in the head with a friend's gun in July 2014 after the local V.A. hospital cut his opioid dose. "SORRY I BROKE INTO YOUR HOUSE AND TOOK YOUR GUN TO END THE PAIN!" he wrote in a note to his friend. "FU VA!!! CAN'T TAKE IT ANYMORE."
Keller's dose reduction seems to have been part of the department's so-called Opioid Safety Initiative, which began in October 2013. A Veterans Affairs "fact sheet" brags that the program reduced the number of patients receiving opioids by a third. According to a V.A. analysis, "opioid discontinuation was not associated with overdose mortality but was associated with increased suicide mortality."
Lamb says the medication he uses to control his pain, fentanyl patches supplemented by hydromorphone pills, is "the difference between wanting to put a bullet in your brain and enjoying life." Despite the huge improvement opioids have made for him, Lamb had a hard time finding someone to continue his treatment after his doctor curtailed his pain practice in 2017. Most physicians in his area "explicitly state they do not do medication management," he says. "I've been having lots and lots of trouble finding another physician. If I can't find one, the natural physiological consequences of severe pain will kill me."
Kertesz says "our focus on pill control" is driven partly by "a recognition that there was a failure to prescribe carefully" but also by "institutional and legal interests seizing on what looks like a simple answer to a complex problem," heedless of the human costs. "We're engaged in a stampede that is trampling people to death," he says, "and those people need to be protected."
Lauren Krisai, a senior policy analyst with the Justice Action Network (and formerly director of criminal justice reform at the Reason Foundation), provided research assistance for this article.
This article originally appeared in print under the headline "America's War on Pain Pills Is Killing Addicts and Leaving Patients in Agony."


Show Comments (185)