NIH Awarded More Than 56,000 Grants in 2020. Just 2 Percent Were for Studying COVID.
More evidence that the public health bureaucracy dropped the ball when a once-in-a-generation pandemic hit.
During the first year of the COVID-19 pandemic, the federal government approved an unprecedented amount of emergency spending in response to a new and poorly understood public health threat.
But the federal government's agency dedicated to actually studying public health threats was slow to respond.
In fact, just 2 percent of the more than 56,000 grants issued by the National Institutes of Health (NIH) during 2020 went to projects studying COVID-19, even as the virus killed thousands of Americans and ransacked the global economy. That's the conclusion of a new study from researchers at Johns Hopkins University and Penn State University that's been accepted (but not yet peer-reviewed or published) by The BMJ, a Britain-based medical journal.
"In the first year of the pandemic, the NIH diverted a small fraction of its budget to COVID-19 research," the researchers conclude. "Future health emergencies will require research funding to pivot in a timely fashion and funding levels to be proportional to the anticipated burden of disease in the population."
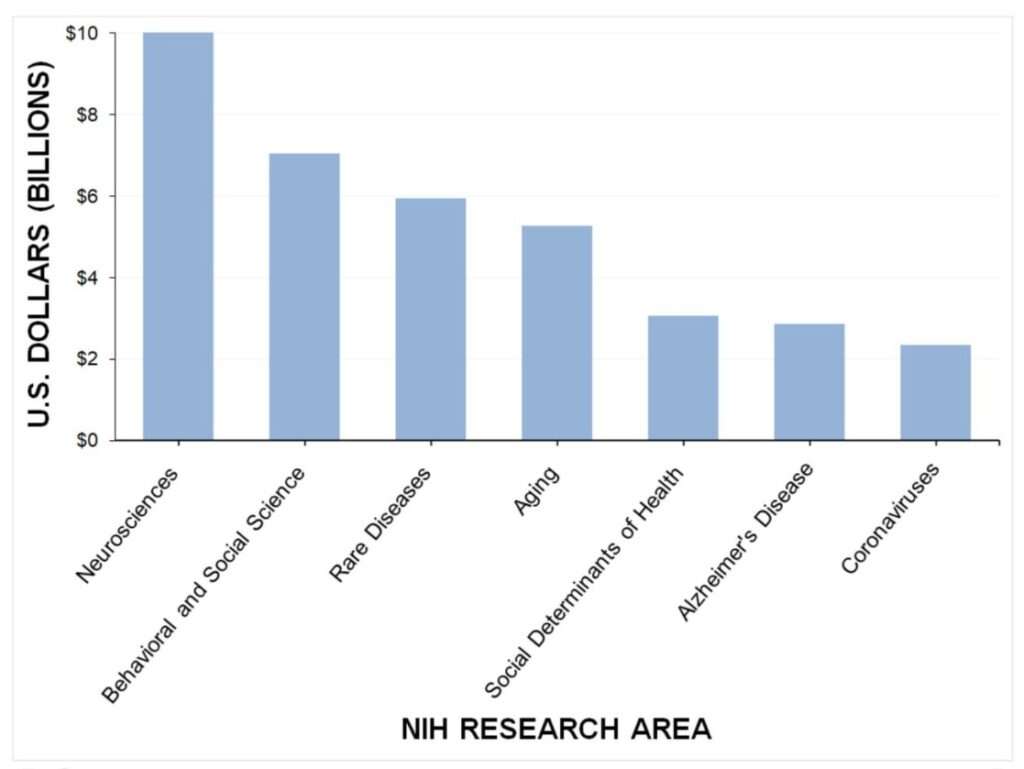
The 1,108 grants awarded for studying COVID-19 accounted for just 5.3 percent of the NIH's $42 billion budget in 2020, according to the report. The NIH dedicated significantly more funding toward behavioral and social science research than coronaviruses during 2020. Studies of rare diseases received about 2.5 times as much funding as coronavirus research, while research into aging got more than twice as much funding.
The COVID-19 research that was funded took a while to get approval. Researchers found that the average time it took for the NIH to approve a COVID-related project was 151 days, with most funding not delivered until the final months of the year.
"The lack of rapid clinical research funding to understand COVID-19 transmission may have contributed to the politicization of the virus," the researchers argue in the paper. "Some of the most basic questions that were being asked of medical professionals in early 2020, such as how it spreads, when infected individuals are most contagious, and whether masks protect individuals from spreading or getting the virus, went unanswered. In the absence of evidence-based answers to the common questions the public was asking, political opinions filled that vacuum."
The study should raise more serious questions about the public health bureaucracy's ability to respond quickly to a developing crisis. For years, the NIH was frequently criticized by figures like Sen. Rand Paul (R–Ky.) for funding wasteful studies that fed cocaine to Japanese quail and nicotine to zebrafish. But when former President Donald Trump proposed cutting the NIH budget by $4.5 billion in 2019, the agency's defenders fretted that the public would miss out on future "ideas and breakthroughs" that would have been generated with those grants.
The COVID-19 pandemic offered a real-world opportunity for the NIH to prove its value. Like the other aspects of America's public health bureaucracy—the Centers for Disease Control and Prevention and the Food and Drug Administration—the NIH seems to have failed that test.
By comparison, a private-sector effort that started from scratch at the beginning of the pandemic was able to invest $50 million in COVID-19 research during 2020. The so-called Fast Grants program was a joint effort of Tyler Cowen, an economics researcher at George Mason University; Patrick Collison, co-founder of Stripe, an online payment platform; and Patrick Hsu, a scientist at the University of California, Berkeley. Nature reported in August 2021 that 67 percent of grant recipients "said their research wouldn't have been possible without a fast grant, and about one-third said it accelerated their work by months."
Fast Grant applications were designed to be completed in less than an hour, with funding decisions made in two days and money delivered within a week.
That stands in stark contrast to the timeline for NIH grants. "From the beginning, the institutional response [to COVID-19] has been lethargic," wrote Cowen, Collison, and Hsu in a June 2021 blog post reviewing their project. "We found that scientists—among them the world's leading virologists and coronavirus researchers—were stuck on hold, waiting for decisions about whether they could repurpose their existing funding for this exponentially growing catastrophe."
Specifically, they pointed to the fact that NIH grant applications require three phases of review by as many as 20 different scientists. No one is harmed by a long review process for a project that gives blow to birds, but the COVID-19 pandemic required a speedier response that wasn't possible for creaky government bureaucracies. "It is difficult for these bodies, such as the NIH, to adapt as circumstances change," the trio concluded.
The new research from Johns Hopkins and Penn State seems to confirm what Cowen, Collison, and Hsu were seeing on the ground as the pandemic hit. The public health bureaucracy's failure to rapidly respond to a once-in-a-generation crisis likely slowed crucial research, left scientists in the dark about how the coronavirus spreads, and created space for misinformation to reign.
We could have followed the science—if only the bureaucrats weren't getting in the way.
Editor's Note: As of February 29, 2024, commenting privileges on reason.com posts are limited to Reason Plus subscribers. Past commenters are grandfathered in for a temporary period. Subscribe here to preserve your ability to comment. Your Reason Plus subscription also gives you an ad-free version of reason.com, along with full access to the digital edition and archives of Reason magazine. We request that comments be civil and on-topic. We do not moderate or assume any responsibility for comments, which are owned by the readers who post them. Comments do not represent the views of reason.com or Reason Foundation. We reserve the right to delete any comment and ban commenters for any reason at any time. Comments may only be edited within 5 minutes of posting. Report abuses.
Please to post comments


Is it once in a generation if we keep saying we're going to lockdown again if cases go up?
Seriously, we could keep doing this for 5 more years then the next generation of schoolkids can live through draconian restrictions and masking idiocy too, every time someone gets the sniffles.
first google hit of what I'm talking about: https://www.dailymail.co.uk/news/article-10625773/Fauci-warns-America-face-COVID-lockdowns-cases-tick-again.html
Finally a proven way of earning money online. Yes! you can earn more than you think only by working just a few hours from home regularly. I have been doing this job for like a few weeks and my last weekly payment was exactly 2537 dollars.
See More Information Here… http://jobscash.tk
Finally a proven way of earning money online. Yes! you can earn more than you think only by working just a few hours from home regularly. I have been Haz doing this job for like a few weeks and my last weekly payment was exactly 2537 dollars.
See More Information Here…Visit Here
Any further attempts at lockdown should be met with the removal and incarceration of the people who attempt it.
Finally a proven way of earning money online. Yes! you can earn more than you think only by working just a few hours from home regularly. I have been doing this job for like a few weeks and my last weekly payment was exactly 2537 dollars.
See More Information Here… Visit Here
"once-in-a-generation pandemic"
Look, the important thing is that a once-in-a-generation pandemic did not cause Koch-funded libertarians to reconsider their demand for unlimited, unrestricted immigration.
#CheapLaborAboveAll
At least Mr. Koch is sticking to his principles, and isn't giving in to the cancel frenzy to pull out of Russia:
https://www.vanityfair.com/news/2022/03/charles-koch-keeping-business-russia
>>likely slowed crucial research, left scientists in the dark about how the coronavirus spreads, and created space for misinformation to reign.
so, worked to plan.
They weren't in the dark so much, as they were simply refusing to see the light.
They saw five lights.
And three seashells.
Maybe the fact that there were 56,000 grants should be more concerning than the 2 percent that went to COVID.
In no way could they have possibly given any real consideration to all of them.
56,000 / 260 = 215 grants per day
(ignores holidays and vacations, assumes no overtime)
According to NIH, they had more than 25,000 reviewers in 2019. It has been a while since I was in academia, but that number rings true. Serving on NIH review panels is a pretty common activity for academic researchers once they reach a certain point in their careers. It's hard work, but each grant application does get reviewed by multiple reviewers at a standard that I'd wager most observers would consider to be reasonably thorough.
It's not a perfect process by any stretch, and one can have a lot of problems with the budget, its priorities, and the number of grants, not to mention whether NIH should exist at all. However, in terms of transparency and deliverables, the NIH grant review process is one of the few parts of government that more or less works well.
And based on what objective measures do you believe it "works well"?
Reviewing a grant is hard work? From some of the grants I've seen get funded, it looks more like the reviewers were tossing darts at a board. That's the only way I can explain grants studying the sex lives of snails or whether drinking heavily is bad for you.
"NIH Awarded More Than 56,000 Grants in 2020. Just 2 Percent Were for Studying COVID."
In fairness, they already spent a bunch of grant money creating COVID, do they really have to fund studying it too?
Getting new variants to come out on schedule doesn't just happen.
lolword
"We'll have to get Dr. Science Fauci to sign off on the animal testing portion, but I'm sure that will be no problem."
This is a nice application, but we see you don't have any experience studying COVID-19.
I am not sure this is any more of a story than that there aren't a lot of women in crab fishing - you can only issue grants to people who are applying for them and meet whatever your minimum standards for rigor are.
If no one is doing that, what's a grant agency supposed to do?
Agreed. This is really a clickbait article. Grants take time to be awarded, to be funded, and to actually have the work done. And a large amount of the work is for basic research - not translational work that could result in a cure. It's the basic research of years' past that allowed us to come up with a vaccine so quickly. You can complain about how grant writing/awarding is done, but it's a little hypocritical to complain that the NIH didn't have a knee-jerk reaction to COVID, especially when Austrian economists complain that the government shouldn't be having knee jerk reactions to every dip in GDP.
Found the guy who lives of the governments teat.
It’s probably not in the NIH’s best interests to encourage legitimate study of the “deadly pandemic”.
^This
Hey, they already had fish bowl cleaner and horse paste cures. No need to spend needlessly.
It's good to see at least one federal agency that is forward-looking.
You don't always want to be preparing to fight the last (previous) war.
More evidence that the public health bureaucracy dropped the ball when a once-in-a-generation pandemic hit.
My Grandma was born right before the 1918 pandemic. My kids' Grandparents were born before both the 1957 pandemic and the 1968 pandemic. Two of my kids were born before the 2009 H1N1 Pandemic.
I remain dubious about the "once-in-a-generation" claim predicated on an organization that's proven itself incompetent even at handling its own balls during *any* pandemic.
25% of children that died from covid miraculously didn't die from covid.
https://www.washingtonexaminer.com/news/reported-pediatric-covid-19-deaths-plummet-24-after-cdc-fixes-coding-logic-error
Can it get any worse for the CDC?
It's almost like government funded research is pointless because the private sector actually incentivizes the things we want. We actually don't need the NIH or ARPA-E or most of the other pointless research departments.
Who will study transgenderism in shrimp of taxpayers won't pay for it?
#defundNIH
re: "while research into aging got more than twice as much funding"
As it should be. Most of us will eventually get covid and some fraction of us will have non-trivial reactions to it. ALL of us will get old, suffer and eventually die from that.
Some of the other criticisms were valid. The one about aging research was not.
Some of the other criticisms were valid. The one about aging research was not.
Disagree. Take all the progress into anti-aging research multiply it by 10 and you still won't produce 1:10th the effective lifespan increase of eliminating sleep. And that's not counting all the ancillary benefits that would trickle down to cognitive science, brain trauma, etc., etc.
We already know that our lifespan is pretty solidly capped by several biological forces that would render us inhuman to thwart even without actually extending our lives. OTOH, there are actual humans who sleep less than half the amount of time most of the rest of us do with no loss of any cognitive, or other, function.
Not an either/or proposition, just that there is no one solution, much less a primary single source for the the one solution.
I'm going to apply for a grant to study the impact of climate change on the vaping epidemic.
Grant applications start being prepared a long time before they're granted. A scientist develops interest in a scientific question before, often long before, they put in for a grant on it. The open secret about grant applications is that the work for the project is almost completed before the grant for it is solicited, which means the scientist had to have been working on it for quite some time beforehand. There simply is no way to have a lot of projects be conceived in time to react to a phenomenon like this coronavirus pandemic unless you allow a lot of vague-interest-based grants that will result in a high proportion of bull shit.
Agreed. And even if it were a new project, it would probably be more than a year for the grant to be funded and the work to actually be done.
There simply is no way to have a lot of projects be conceived in time to react to a phenomenon like this coronavirus pandemic unless you allow a lot of vague-interest-based grants that will result in a high proportion of bull shit.
To be fair, this should probably say high*er* proportion of bullshit. Moreover, still baked into the problem despite your point is that the government is still holding the brass ring or the carrot. They just aren't holding it as closely to the donkey's nose as the article portrays.
Eric - This is a ridiculous criticism.
First and foremost, NIH funding and NIH funded researchers are orientated towards basic research. They aren't in the same position as industry scientists with regards to rapidly developing, testing, and delivering new therapeutics. Even if they had been given tons of monies quickly, they would be hard-pressed to produce something useful in a time frame that would alter the course of a pandemic.
Second, NIH funding cycles are yearly. Researchers were already engaged in approved research and to suddenly toss those research programs out the window would be extraordinarily wasteful. Related, most NIH researchers work outside the field of infectious diseases. They can't turn their expertise on a dime no matter the funding.
Third, it's not all about the short term. Turning cancer and cardiology researchers into epidemiologists overnight, impacts progress in these fields. Given that over half of deaths are due to cancer or heart disease, delaying new future therapeutics based on current research, could end up costing more lives in the long term than it saves in the short term.
Finally, the United States did do an excellent job with Operation Warp Speed. The federal government essentially got into bed with industry and underwrote the risks for developing the vaccines. That is, we put our resources behind industry, which, unlike the NIH, is specifically tooled to develop vaccines and therapeutics.
Overall your criticism is scurrilous and betrays an ignorance of how biomedical research operates.
(As for Tyler Cowen, the less heard from this quack the better.)
Not to defend Eric too vociferously but;
Third, it's not all about the short term.
...
Overall your criticism is scurrilous and betrays an ignorance of how biomedical research operates.
It is about the short term. You can't teleport before you can walk and trying to teleport before you can walk leaves you grossly unprepared for teleportation in the environment of walkers... and drivers... and pilots... and astronauts. Further, as I point out above, the NIH dictating long term research goals is still the NIH dictating long term research goals.
We've been through this with computers and there's a false assumption that the research *must* be done. I've powered down enough COBOL and Fortran systems with math co-processors and spun up enough FPGA rigs that are no longer profitable to confirm that it happens all. the. time. Like if we nuked ourselves back to the Stone Age tomorrow, we wouldn't skip the invention of the slide rule and go straight to re-establishing semiconductor production. That's not to say that 50 yrs. of cancer research hasn't done any good, or that cancer and cardiologists should be able to turn on a dime any more than coal miners should be able to learn to code, but that the notion that "It's not all about the short term." contains unknowable assumptions about the long term and, more importantly, who should (and shouldn't) be making those assumptions.
"When railroading time comes you can railroad—but not before." - Heinlein
This is a poorly researched and thought-out article and opinion. The Federal fiscal year, under which NIH operates it's annual funding cycle, runs from Oct 1 to Sept 30 each year. The first COVID cases reported in the US were February 29, 2020, five months into the fiscal year. That left 7 months in FY20 to transfer funds to COVID research that were designated for other purposes, put out the call for proposals, review them, and then fund them. That NIH was able to put $2 billion of its total funding toward COVID in that timeline is actually an achievement. Especially given the drastic cuts that the Trump administration was attempting to inflict upon NIH at the time.
While it's true that Trump did call for actual cuts in the NIH budget, the NIH budget increased steadily during his presidency. For the 30+ years I've been in science, every time someone has tried to cut the proposed *rate of increase* (never mind proposing *actual* spending cuts), the proposals almost always get described as "catastrophic" or "draconian".
FWIW, the last time the NIH budget was "drastically" cut was in 2013, and it was only a 5% cut. Actual cuts to NIH budgets are rare, and aside from that single 5% cut, none have been more than around 1% in the last few decades. The total NIH budget has roughly doubled in that time, even after adjusting for inflation. I love science, but there is no special interest group with a greater sense of entitlement than NIH-funded scientists.
WOW... you are a real piece of work. All of your "facts" are absolute hogwash. NIH funded scientists are "entitled"?! Do you even know the definition of that word? Don't answer that--because you don't. Please educate yourself, if you're even capable of that. What are your credentials? Do you have a PHD? Have you spent the last 25 years funding YOUR OWN SALARY like every NIH funded scientist in the field is forced to do?!? Please never speak another word again, your ignorance is absolutely staggering.
Yes: they believe that somehow taxpayers have an obligation to fund their research.
If they are "NIH funded", they obviously aren't "self-funded".
A lot better than yours, I assure you.
Thanks for putting your arrogance and sense of entitlement on full display.
FWIW, I received my first NIH grant about 30 years ago. I'm in industry now, and I don't miss the grant treadmill one bit. The grant process is not an easy process. Your emotional, condescending reply seems to support my point about entitled attitudes. "How dare anyone without a PhD question NIH budgets or hold a critical opinion about my peers! Silence, commoner!"
Excellent response, you are 100% correct.
Just in case there are RepubliQQQlans around... who was president in 2020?
Following the science.
This is an OUTRAGEOUSLY ignorant and misleading article written by someone who has zero knowledge of the field of science research. Cancer is grossly UNDERFUNDED by NIH and neuroscience is grossly OVERFUNDED. This is extremely reminiscent of bioterrorism because it was a 'hot topic' for a short period of time a decade ago. So covid research should be over-funded because pop culture thinks we should throw all of our money into something that ALREADY HAS THREE VACCINES!!! WOW. Stop with this baseless propaganda, it's pure ignorance. Go interview 20 scientists who work in the field who are having their funding cut and salaries cut because they're trying to cure CANCER on a shoestring budget. Mr. Bohem should literally be fired. You're a hack, you don't have a PHD and you have less than zero knowledge of what you're lamely attempting to speak about here. Zero educated sources to support this article. Covid has been around for two years--cancer and autoimmune disorders have been around for CENTURIES and are FAR, FAR more important and impactful than a temporary pandemic that we literally have under control. This article is the very definition of fake news. It's literally unbelievable. Before you ever have an 'opinion' on this topic (which is all this is) you should educate yourself. The fact that this article showed up on The Drudge Report is literally a criminal act. I hope you never pen another article ever again, on any topic whatsoever. This is despicable on multiple levels.
If government funding for scientific research is justifiable at all, it is justifiable only to fund basic research that otherwise wouldn't be financed by the private sector.
There is massive private spending on cancer research because cancer treatments are highly valuable; therefore, there is no need for public funding.
There is little private spending on neuroscience research because there are few practical applications. That's why government funds it.
But greedy, entitled, immature academic researchers look down their noses at private industry.
@ JS555333 I agree the article is ignorant about how NIH works, and it is pretty worthless as anything except clickbait, but you do science no favors with your condescension and contempt for people whose pockets are being reached into to pay for NIH grants. It's possible that you are a terrific scientist, but you probably should get some communications training before publicly engaging the citizenry on policy questions.
No, what it is actually evidence of is that COVID is a fairly run of the mill virus that doesn't require a lot of extra study, that the federal bureaucracy knows this full well, and that all the hype about COVID is politically motivated fear mongering.
Pretty sure they don't want the scrutiny.