Vaccines Don't Save Lives. Vaccinations Save Lives.
Especially if the COVID-19 inoculations are deployed speedily and accepted widely.

In less than a year since the COVID-19 pandemic began, several safe and effective vaccines against the coronavirus are apparently on track to be approved and made available later this month. This spectacular achievement is in large part due to the federal government's Operation Warp Speed program that incentivized pharmaceutical companies to rapidly develop and deploy these vaccines. Operation Warp Speed's chief science adviser Moncef Slaoui told The Washington Post this morning that he expects there will be enough COVID-19 vaccine to immunize every American by June 2021. Vice President Mike Pence said yesterday that vaccine distribution could begin during the week of December 14.
But as Emory University infectious disease researcher Walter Orenstein reminds us, "Vaccines do not save lives. Vaccinations save lives." The question of just how many infections, hospitalizations, and lives lost could be averted by the rollout of the COVID-19 vaccination campaign is at the heart of a new modeling study in Health Affairs by a team of Harvard and Yale researchers led by infectious disease physician Rochelle Walensky.
It's great to have highly effective vaccines, but as the researchers observe, "How well a vaccine program 'works' will also depend on how quickly it can be manufactured, how efficiently it can be distributed to locations in greatest need, how persuasive health messaging can be in promoting public acceptance, and how consistently the public can adhere to the many complementary prevention strategies (e.g., masks, hand-washing, distancing) to limit the spread of the virus."
To get at the question of how well the upcoming COVID-19 vaccine campaign might work, the researchers set up a heavily caveated model that seeks to take into account the relative efficacy of vaccines (25, 50, 75, and 90 percent) that are preventive, or severity reducing (disease modifying), or a composite of both. The model also takes into consideration the pace (speed of deployment) and coverage (extent of vaccine uptake) as they interact with various epidemic severity scenarios. The researchers also consider various lag times for the vaccines to become fully effective. For simplicity the simulation uses a population of 100,000 people.
In their base case, the pace is 0.5 percent of the population is vaccinated daily and they assumed an eventual coverage of 50 percent of the population. They defined three different epidemic severity scenarios based on basic reproduction numbers, that is, the average number of people to which an infected person will transmit the virus, ranging from a best case of 1.5 to a baseline case of 1.8 to a worst case of 2.1 people. In the best case scenario, people are keeping the basic reproduction number lower by adhering to social distancing, mask wearing, and other preventive practices. The higher number is associated with greater crowding indoors as the weather grows colder. They also sketch out a scenario in which the basic reproduction number is 1.2 cases per infection. As it happens, that appears to be close to the current nationwide level.
Their baseline scenario assumes an epidemic basic reproduction number of 1.8. With no vaccinations, more than 61,000 people out the population of 100,000 would become infected within six months. Cumulative deaths would reach 2,725 and hospitalizations would peak at 1,780 people. The researchers then assume that 50 percent of people are inoculated with a composite vaccine that is 50 percent effective after 42 days at preventing—as well as reducing—disease severity. In that case, total infections drop to around 37,000 (32,000 unvaccinated and 5,000 vaccinated). Cumulative deaths among the unvaccinated fall to 1,430 and to only 16 for those who are vaccinated. Peak hospitalization drops to 962 people.
Keep firmly in mind that these calculations are not predictions about what will actually happen in the coming months. They are designed to provide some insight on how the interaction of the speed of deployment, vaccine uptake, and the severity of the epidemic could affect the trajectory a vaccination campaign during the COVID-19 pandemic.
In a scenario with a six month time horizon (say, by this June) in which the basic reproduction number is 1.5, the vaccine is 90 percent effective, 1 percent of the population is vaccinated daily, and 90 percent are eventually vaccinated, infections are cut by more than 90 percent below what they would have been without a vaccine.
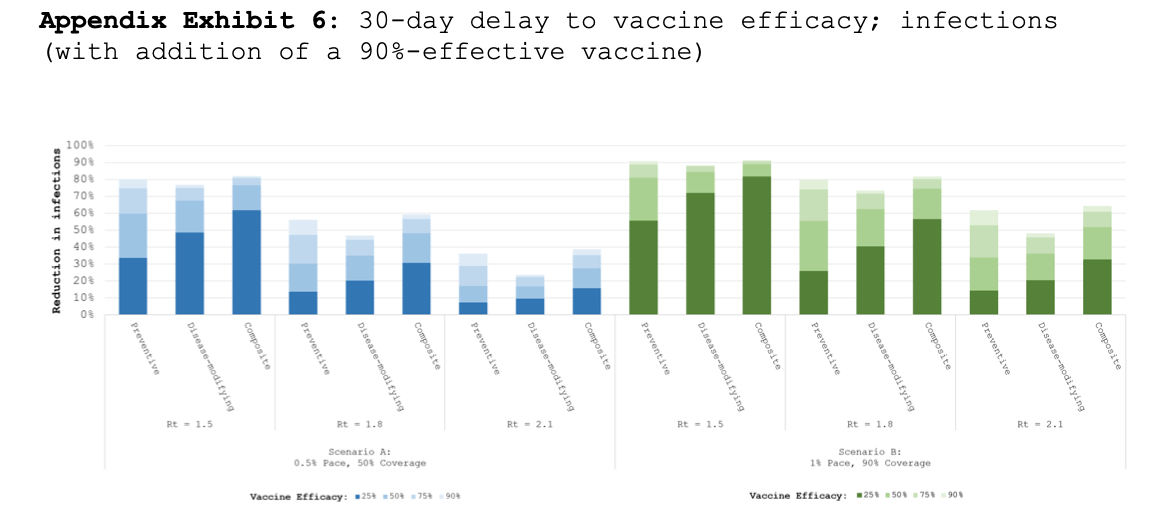
If the epidemic is more severe, with a basic reproduction number of 2.1, then infections over six months in that scenario are only reduced by a little over 60 percent. The basic reproduction number for the COVID-19 pandemic now depends largely on the actions we choose to take—avoiding crowded indoor spaces, mask wearing, and proper hygiene—to slow the trajectory of the pandemic for the next several months as the vaccines are rolled out. While the highly effective vaccines that appear to be in the pipeline are critical to ending the pandemic, the researchers point out, "the benefits of a vaccine will decline substantially in the event of manufacturing or deployment delays, significant vaccine hesitancy, or greater epidemic severity."
With respect to vaccine deployment, Robert Redfield, director of the Centers for Disease Control and Prevention, testified last September in a Senate hearing that it would take about $6 billion to adequately fund the speedy distribution of the coronavirus vaccines. A bipartisan $908 billion stimulus plan proposed today in Congress would authorize $16 billion in health care funding that would allocate some spending for coronavirus testing and tracing and vaccine distribution.
Extensive vaccine hesitancy would stymie the development of real herd immunity to the coronavirus. Most researchers now believe that achieving the herd immunity threshold for COVID-19 would require that close to 60 to 70 percent of the population will have to have been infected or vaccinated. The good news is that a poll released in early November by the STAT biomedical research newsletter and the Harris Poll reported that 63 percent of Americans responded that they would get inoculated if the COVID-19 vaccines were 90 percent effective. In clinical trials, the Moderna and the Pfizer/BioNTech vaccines are more than 90 percent effective in preventing infections. My hope is that as vaccine-hesitant Americans see most of their neighbors getting inoculated, that they too will choose to take the responsibility to protect themselves and vulnerable others from the COVID-19 scourge.
Ultimately, this modeling exercise suggests that millions of infections, hundreds of thousands of hospitalizations, and tens of thousands of deaths can be averted in the coming six months if we keep the COVID-19 epidemic relatively under control and persuade our neighbors to take advantage of this amazing biomedical achievement.


Show Comments (112)