The Authors of the CDC's Opioid Prescribing Advice Say It Has Been 'Misimplemented' in a Way That Hurts Patients
The CDC decries abrupt, involuntary dose reductions and patient abandonment without acknowledging its responsibility for those unintended but foreseeable consequences.

In a New England Journal of Medicine commentary published today, the authors of the opioid prescribing guidelines that the U.S. Centers for Disease Control and Prevention issued in 2016 reiterate the agency's recent warning that it does not recommend abrupt or nonconsensual tapering for patients who are already taking high doses of narcotic analgesics for chronic pain. "Unfortunately, some policies and practices purportedly derived from the guideline have in fact been inconsistent with, and often go beyond, its recommendations," write Deborah Dowell, Tamara Haegerich, and Roger Chou. Those policies and practices, they say, include "inflexible application of recommended dosage and duration thresholds and policies that encourage hard limits and abrupt tapering of drug dosages, resulting in sudden opioid discontinuation or dismissal of patients from a physician's practice."
Dowell, Haegerich, and Chou warn that patients forced to reduce their doses "could face risks related to withdrawal symptoms, increased pain, or unrecognized opioid use disorder" and "if their dosages are abruptly tapered may seek other sources of opioids or have adverse psychological and physical outcomes." They also worry that doctors are responding to the CDC's advice about the potential risks of opioids by "dismiss[ing] patients from care" or declining to prescribe opioids at all, "even in situations in which the benefits might outweigh the risks." Dowell et al. say "such actions disregard messages emphasized in the guideline that clinicians should not dismiss patients from care, which can adversely affect patient safety, could represent patient abandonment, and can result in missed opportunities to provide potentially lifesaving information and treatment." And they note that the guidelines have been improperly applied to "patients with pain associated with cancer, surgical procedures, or acute sickle cell crises."
The CDC's recognition that misinterpretation of its guidelines has resulted in needless suffering, patient abandonment, and "adverse psychological and physical outcomes" (including suicide) is welcome, if overdue. "This article should allay anxiety among physicians who prescribe responsibly for patients with chronic pain," says Sally Satel, a Washington, D.C., psychiatrist who helped organize a March 6 letter to the CDC in which hundreds of health professionals and addiction specialists, including three former drug czars, expressed concern about the unintended consequences of the CDC's advice. "No longer can any clinician, insurer, health care system, or pharmacist claim 'the CDC Guideline says' when it comes to tapering or discontinuation."
Stefan Kertesz, a University of Alabama at Birmingham pain and addiction specialist who worked with Satel on the letter to the CDC, was also heartened by the NEJM article. "We needed CDC and its guideline's authors to do precisely what they have done, which was to speak with vigor and clarity to the pressing ethical concern we laid out in our letter," he says. "In affirming that the guideline did not call for hard dose cutoffs and forced tapers, the guideline's authors have effectively called for recalibration of policies by insurers, by Medicaid authorities, and by agencies that have set 'the number of patients above a given dose' as the primary indicator of bad care."
The letter to the CDC included testimony from hundreds of patients who have suffered the consequences of that ham-handed approach. "The trauma to patients who have been living in terror these past three years nearly broke my heart many times," Kertesz says. "The only possible step has been for people familiar with the nexus of science and health policy to speak openly about the problems we have seen, and to trust that most people ultimately want to do what's right."
Yet Dowell et al. conspicuously fail to take any responsibility for the unintended but foreseeable harm caused by their advice. When a document is as widely misconstrued as the CDC's guidelines have been—by insurers, regulators, legislators, pharmacists, and law enforcement agencies as well as clinicians—it is fair to ask how the authors left themselves open to misinterpretation.
According to the guidelines, "Clinicians should use caution when prescribing opioids at any dosage, should carefully reassess evidence of individual benefits and risks when considering increasing dosage to ≥50 morphine milligram equivalents (MME)/day, and should avoid increasing dosage to ≥90 MME/day or carefully justify a decision to titrate dosage to ≥90 MME/day." The implication is that doses of 90 MME or more per day are rarely, if ever, medically justified.
It is hardly a stretch for physicians with patients who exceed this arbitrary threshold, including patients who have been functioning well on high doses for years, to worry that they will be perceived as practicing outside the bounds of proper medical care. Given the scrutiny that regulators and law enforcement agencies such as the Drug Enforcement Administration (DEA) have been applying to doctors in response to the "opioid epidemic," prescribing practices portrayed as extreme and dubious by the CDC are apt to attract unwelcome attention that could jeopardize a physician's livelihood and liberty.
"We still, unfortunately, have physicians who worry about capriciousness on the part of the DEA," Satel notes. "That is the next step in efforts to ensure that doctors can continue to serve pain patients who have been benefiting from opioids." While "the DEA does indeed have a job to do," she says, "doctors are confused about what could make them a target."
How doctors respond to anti-opioid pressure will depend on how they weigh their duty to patients against their personal risk. In this context, forced tapering and abandonment were predictable outcomes, even though the CDC guidelines say doctors should reduce doses only when the risks outweigh the benefits and describe the process as collaborative and consensual.
"Clinicians should empathically [sic] review benefits and risks of continued high-dosage opioid therapy and should offer to work with the patient to taper opioids to safer dosages," the guidelines say. "For patients who agree to taper opioids to lower dosages, clinicians should collaborate with the patient on a tapering plan."
Dowell et al. complain that "the guideline has been misimplemented," saying "policies invoking the opioid-prescribing guideline that do not actually reflect its content and nuances can be used to justify actions contrary to the guideline's intent." But those nuances were bound to be lost amid the fear and anxiety caused by the government's crackdown on prescription pain relievers.
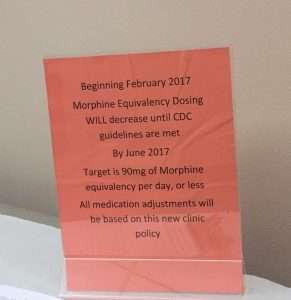
Notwithstanding Dowell et al.'s disavowal of "hard limits and abrupt tapering," that is what happened across the country after the CDC guidelines came out, as reflected in this sign at a doctor's office in Washington state. "Beginning February 2017," it says, "Morphine Equivalency Dosing WILL decrease until CDC guidelines are met by June 2017. Target is 90mg of Morphine equivalency per day, or less. All medication adjustments will be based on this new clinic policy."
While decrying involuntary and precipitous tapering, Dowell et al. present the general decline in opioid prescribing as a sign of progress. "Although outpatient opioid prescribing had been declining since 2012," they write, "accelerated decreases—including in high-risk prescribing—followed the guideline's release." Yet the continuing drive to reduce the volume of opioids prescribed in the United States has encouraged doctors, insurers, and policy makers to target patients on high doses, who consume a disproportionate share of the total. Kertesz emphasized that point at a recent conference in Charleston.
Dowell et al. do not acknowledge the downside to the decline in opioid prescribing, which has been accompanied by a surge in opioid-related deaths as both patients and nonmedical users turn to the black market, where the drugs are much more dangerous because potency is highly variable and unpredictable. Nor do they question their emphasis on the 90-MME threshold, which is scientifically problematic for several reasons. It assumes that analgesic effect corresponds to overdose risk and that different opioids can be reliably compared to each other based on fixed ratios. It ignores numerous factors that affect how a patient responds to a given dose of a particular opioid, including obvious considerations such as the patient's weight, treatment history, and pain intensity as well as subtler ones such as interactions with other drugs (which can suppress or amplify an opioid's effects) and genetically determined differences in enzyme production and opioid receptors.
"Policies should allow clinicians to account for each patient's unique circumstances in making clinical decisions," Dowell et al. write. The CDC's 90-MME threshold, however it was intended, has in practice encouraged a much less discriminating approach, one that sacrifices patients' welfare for the sake of conforming with the perceived demands of the federal government.
"The CDC bears full responsibility for how these arbitrary dose levels are being implemented throughout the country and the consequences for the people in pain," Lynn Webster, a former president of the American Academy of Pain Medicine who signed the March 6 letter to the CDC, told me last year. "I said at the time when they were proposed that if something comes from the CDC as a guideline, it is more than a guideline. It will be interpreted basically as a level of dosing that if you exceed [it], then you are at legal jeopardy."
Editor's Note: As of February 29, 2024, commenting privileges on reason.com posts are limited to Reason Plus subscribers. Past commenters are grandfathered in for a temporary period. Subscribe here to preserve your ability to comment. Your Reason Plus subscription also gives you an ad-free version of reason.com, along with full access to the digital edition and archives of Reason magazine. We request that comments be civil and on-topic. We do not moderate or assume any responsibility for comments, which are owned by the readers who post them. Comments do not represent the views of reason.com or Reason Foundation. We reserve the right to delete any comment and ban commenters for any reason at any time. Comments may only be edited within 5 minutes of posting. Report abuses.
Please to post comments


Clearly, the federal government is abusing its authority to regulate the practice of medicine, one almost wish the Constitution hadn't delegated the feds such a power.
/sarc
Get the government out of the way of the patient/doctor relationship by putting the government in total charge of the entire process. Think of it as stepping from in-between and putting both in a big bear hug.
Tapering is good medical practice and these extremist doctors need to stop pretending that any level of pain is unacceptable. Tough it out or risk getting addicted to heroin; the choice is clear.
So what if a person is addicted to opioids? That is between them and the doctor. All the government has done is encourage one-size-fits-all command style solutions that mean people with legitimate need are lumped in with addicts.
And by the way, this has had further cast down effects. Providers are so scared that they will get flagged, that they avoid prescribing any opioids. My wife broke her hand, and they gave her like 3 days of pain pills, and she was suffering for at least a week after that. My daughter had an appendectomy and they had her using ibuprofen to deal with the pain (unsuccessfully). In both cases, their recovery would have been much easier, and likely would not have led down the road to addiction, but these policies mean they have to do without.
In addition to the industry reaction to this opioid hysteria, it has also cascaded into additional wasteful nonsense. When my wife broke her hand, I dropped her off at home after the hospital trip and went to the local CVS to get her prescription. I had to sit there for 2 hours waiting for the prescription to be filled because the stupid regulations require the opioids to be locked in a safe with a 1 hour timer.
Because some people were abusing opioids, they make it harder for everyone to get them. Because those abusers then resort to the black market and theft, they make it harder for everyone to get them.
And to what end? These policies have resorted in MORE opioid deaths because they have chased people with a problem away from a doctor and to fentynol dealers.
I bet the timer was to deter robberies. But still ridiculous. That must be a state reg. When I had surgery last fall, I only waited about 20 minutes for my opioid prescription.
How does the 1 hour timer work? It can be opened only once per hour? Or, like, you have to tell it to open, and then wait an hour before it does?
Tough it out or risk getting addicted to heroin; the choice is clear.
If it's a choice, THEN LET THE PERSON MAKE A CHOICE. The risk is overblown.
You sound like you need to be put in severe pain then denied any access to opioids or any other painkiller stronger than ibuprofen.
Where is your evidence that tapering is good medical practice? There is none. Tapering hurts patients who are FUNCTIONING in society. Letting the government decide who gets a medication that gives patients their health and allows them to be contributing members of society is unconstitutional. The risk of addiction for chronic pain patients is less than .5 percent .
I wanted to start this by saying "Moron:; but I'll temper my comment: Dolt-.
We do not ever advocate these as first, second or even third line therapies. Maybe 20 years ago some did.
Now: we reserve these meds for maybe 2% of the population -at doses near or above CDC where as the most recent data suggests as many as 19% of the population live with moderate to severe pain 6days a week or more. So less than 5 million people receive regularly prescribed opioids-yet 50 million could potentially benefit.
Pain accelerates multi-system and neurologic decline; impairs immunity; reduces length and quality of sleep; is a significant cause of older adult social isolation; and, is a major cause of a little problem called mental health disease. Untreated and underrated pain is among the most cited reasons otherwise normal people try illicit drugs.
Before opioid trials the typical patient will see 4-5 physicians who'll try numerous other options before even considering an opioid.
Social media may entitle different points of view, but should be restricted to those who have IQ's over 70. Keep your biases to your self
The science is settled
Careful with that.
MS. Reynolds: very valid point...and by science what exactly is implied?
The science of opioid efficacy? Or lack thereof?
Acute v chronic pain?
The science of central sensitization?
The science of neuro-plasticity?
If so, after 30 years of this I'd like to know where...
How addictive is this stuff, really? Anybody here had an issue with it?
Not very if used properly, by most people. Some are predisposed to it.
Despite all the hysteria, percocet, vicodin, morphine and all the old school opioids have not suddenly become more addictive.
Tanks
APCs
If you take enough for long enough, you will feel really sick if you stop.
Whether one is likely to become a junky is a lot more to do with the individual's predisposition to addictive behavior than anything, I think. Plenty of people can take the drugs while they need them, feel a little sick for a while while they stop and then get on with their lives.
My doctor hadn't intended I withdraw suddenly from tramadol instead of tapering it, but I did because I hadn't expected a month on it to produce an abstinence syndrome. It wasn't unpleasant, it was weird. Sort of a trip in itself. Hyperactivity, lots of introspection and emotion. Might be interesting to go thru that intentionally some time.
However, my friend after 2 months on it described the withrawal as awful.
Well here is where statistics can get one in trouble: populations have differences based on age, sex, genetics and ethnicity (not PC, but true)
It is proposed we are all at risk at some level.
2 issues:
In a nut shell:
younger,
male
smoker
family history of substance abuse (SA)
Personal history of SA
ANY CO-OCCURRING mental health disorder, esp anxiety and PTSD
And:
Some molecules (drugs) may be more problematic than others: Speed of entry to the brain activating reward circuitry is very important; and some opioids in certain patients have a more generalized effect on at risk brains-rather than pain relief, the patient gets a sense more of well-being. That is a major (unrecognized) red flag.
hope that helps
About as addictive as ibuprofen in my experience. When I have rare patches of significantly reduced pain I tend to forget to take my every 12 hours slow release opiate pill. Then it will be like 10 hours after I was supposed to take it and some pain will come back and I'll get those scary, horrible opiate withdrawals - aka a runny nose - and I'll think "oh that's why - I forgot to take my morning opiate pill".
In Dreams and Visions Given to me by Government Almighty, I have received the following Sacred Messages:
Pain-killing drugs are for WUSSIES!!! Mighty Men and Mighty Women will use acupuncture, aromatherapy, Feng Shui and-or Fag Shui, holistic organically-grown rubber mouth-guards to bite down on, and, ultimately, if need be, suicide, to avoid the pain! Anything else is utterly limp-dicked! Are YOU ready to face an Angry Government Almighty, after you die, and you find yourself as a sinner in the hands of said Angry Government Almighty, for having GOTTEN ADDICTED TO CHEMICAL PAINKILLERS on your deathbed?!?! Are you ready to go SOOO far, and RUIN it all, in your last, fleeting moments of weakness?!?!?
This can all be solved with an OTC lung flute.
Thank Yew Unicorn Abattoir!!!
As usual, though, the devil is in the details... An OTC lung flute, blessed by Government Almighty, would be a WUNDERBAR thang!!!
However, if we'd smear some evil-chemical-based painkillers onto the lips-interfacing surface of the lung flute... Who knows HOW MANY addicted souls would have to be ETERNALLY PUNISHED by Government Almighty?!?!
Nonsense. You're supposed to pray the pain away. God will take your pain away if you are truly faithful.
Good thing there is a black market.
Slavery? Check your intersection.
Good thing there is a
black marketunregulated marketplace for the historically marginalized and oppressed.FTFY
I like to buy the historically marginalized and oppressed at a discount whenever possible.
be very very very careful: in most US cities, regardless of what the pill looks like it is likely bogus and made with heroin and or fentanyl-that is the current cause of many of the opioid related deaths-individuals (AKA Prince) getting heroin and fentanyl when he was told it was hydrocodone....
"This article should allay anxiety among physicians who prescribe responsibly for patients with chronic pain,"
Yes, as long as they are prescribing responsibly. Now, there's a large, powerful government agency with the authority to destroy you backed by men with guns with the ability to destroy you who have issued their opinion of what "responsibly" means, but by all means feel free to substitute your own opinion of what "responsibly" means for theirs. I don't see why there should be any problem with this.
(And didn't I make pretty much this same comment a while back when pretty much this same article was posted?)
That was the old site; this is the new site.
"We really didn't mean it! Our fingers were crossed behind us!"
Your tax dollars at work.
Did Reason finally find something that is made worse by bureaucratic and policy-making central planners? Suderman and Poole should write a rebuttal to Sullum's heresy.
"Single-payer" healthcare will solve this. When the Top Men in the government are centrally planning our healthcare, we'll be lucky if we can get a moldy aspirin from them.
And don't plan on biting down on a bullet. Bullets will be banned by the Top Men.
While "the DEA does indeed have a job to do,"
The DEA has many more lives to ruin, and we do not want to get in the way of the DEA's mission to ruin lives.
"acknowledging its responsibility for those unintended but foreseeable consequences"
A foreseen consequence can never be unintended.
They meant every word of what they said, and expected everything that occurred, except MAYBE the backlash.
The people who wrote the guidelines made a pathetic error, and are now whining in self-pity about the public perception of error that they made but are actually not taking full responsibility for it.
Every intervention, whether it's crossing the street or having surgery has benefits, risks, Alternatives, and imponderables. That there was a risk of habituation, IE, addiction, to opioids and too many other drugs was well-known. The feds Force Physicians to provide luxurious and unnecessary dangerous and potentially habituating medication at risk of chastisement and penalty. Now they've done it in reverse and now they are reversing the reverse. This is what happens with top-down medicine. And since no matter what members of the public say, it's going to get worse, it's going to get worse. Watch. Watch.
My perspective is probably rare and relevant. My wife has suffered with CRPS for over 30 years and needs pretty high doses of opioids, along with a bunch of other things, to survive. I have spent much of my career dealing with governmental rules and regulations, and their interpretation.
It boggles the mind that the people who put out the original CDC guidance didn't realize--and weren't told by experienced regulatory hands--that what they viewed as 'guidance' would be interpreted as 'hard compliance requirements', with penalties for violation involving loss of medical licenses, disqualification from Medicare, sanctions on the hospitals or clinics, and perhaps criminal exposure.
Based on 3 decades of experience parsing govt rules, upon a close reading I could tell that was not the intent, but to a person without that experience, or just one whose career is on the line, that kind of fine-grained parsing of texts is not at all adequate.
This was and remains a total cluster-f**k. Some states changed their own licensing rules to conform to the CDC guidelines and that damage will not be undone speedily or totally. And the amount of unnecessary suffering by pain patients will never be known but should rank as one of the great medical catastrophes of the last few decades. And there are now lawsuits working their way through the courts, alleging that a doctor harmed his/her patient by prescribing >50 MME... and that will go on a long time.
Total disaster, and could have easily been avoided. with a few words in the body of the guidance document.
[…] and patient abandonment, have become painfully clear, as the authors of the guidelines finally acknowledged last […]
"I said at the time when they were proposed that if something comes from the CDC as a guideline, it is more than a guideline. It will be interpreted basically as a level of dosing that if you exceed [it], then you are at legal jeopardy."
No kidding. When a government regulatory agency says you need to "carefully justify a decision" that clearly and obviously means "be prepared to justify in court" not merely "use your best judgment" and anyone who thinks otherwise is delusional.
[…] and patient abandonment, have become painfully clear, as the authors of the guidelines finally acknowledged last […]