We've Known for 40 Years How to Help Heroin Users
In the 1970s, New York City and Hong Kong figured out how to help heroin users without red tape or an abundance of experts.
America's current wave of heroin overdose deaths is not without precedent. Between 1969 and 1972, the number of heroin users in America doubled, and no place was hit harder than New York City. Of an estimated half a million heroin users nationwide during the 1970s, some 200,000 lived in NYC, and as many as 650 New Yorkers died annually from overdoses. The way New York City government responded to the crisis remains the best example of how to quickly and effectively scale up medical care for people with opioid use disorders.
While New York Gov. Nelson Rockefeller responded to the rise of heroin by signing the Rockefeller Drug Laws in 1973 and instituting the first—and initially, harshest—mandatory minimum sentences for low-level drug offenders in the history of the U.S., New York City Mayor John Lindsay decided to focus city resources on expanding access to methadone.
Methadone, which we still use today, acts on the same receptors in the brain as do heroin and prescription opioids. Rather than requiring users to quit cold turkey, which often leads to relapse and overdose, methadone scratches the opioid itch with a much milder high. In addition to helping users hold down jobs and obtain housing, methadone and its more modern cousin, buprenorphine, have been shown to reduce opioid mortality rates by as much as 50 percent. People with opioid use disorders can take methadone and buprenorphine indefinitely if they want or need to, and many do.
Lindsay wanted more methadone in New York, and the way he accomplished that will boggle the minds of contemporary public health advocates.
In 1969, after a narrow re-election, Lindsay nominated a man named Gordon Chase to oversee health services in New York City.
A 37-year-old with a bachelor's degree in political science, Chase had worked on budgets in the city's Human Resources Administration and played bit parts in the John F. Kennedy and Lyndon B. Johnson White Houses. But he didn't know anything about health care. The New York Academy of Medicine sent a letter to Lindsay saying Chase was "professionally unqualified" to run the Health Services Administration, and groups around New York echoed their concerns.
But Chase was just as committed to creating a citywide methadone program as Lindsay was. Over the next three years, he launched the largest heroin treatment program in history with the help of physician Robert Newman. Then only a few years out of medical residency, Chase told Newman he wanted him to be "Mr. Methadone" and named him Assistant Commissioner of Addiction Programs.
Newman would have all the resources the city could marshal, Chase said, but the catch was that he had to build a network of clinics faster than any expert thought was wise. According to an interview Newman gave to researcher William White several years ago, medical experts were so horrified by their plan to scale up quickly that Newman asked Chase if maybe they should put the brakes on:
Newman: Every single objection I raised—and I raised objections that I had heard from [other physicians]. They said, "Well, you need six weeks of training, and you need this. You need that. When you open the new clinic, you can't admit more than one or two patients a week for the first whatever."
Every single objection I raised, Gordon's response would be, "Is it really better to leave people on the street to shoot dope who want this treatment that you think is effective?" My bottom line answer to him was, "You're right. We have to do whatever it takes to achieve the goal." Gordon Chase's compelling argument was this: Imagine a woman barging into your office one day telling you her son, a long-term heroin addict, had applied for treatment but was turned away by your program and put on a waiting list because you had no room—and then died of an overdose. He said, "Bob, you tell me what excuse for moving slow you will give this woman that will elicit the response, "Oh, I understand. Of course you had to wait until all the furniture was placed, or of course, you didn't want to burden the new staff with too many patients. My poor son had to die, but at least I understand now that it was for a very good reason." He gave me that speech once or twice until I got it.
So Newman and Chase pushed forward despite concerns that the program was growing too fast. At one point, Newman set up a clinic in a boat anchored at battery park, transporting methadone doses to and from the makeshift center in his son's carriage. The result of their vision was that within three years, New York City was providing methadone to 10,000 patients.
New York City's methadone maintenance program would eventually be handed over to the state government due to budget cuts. But it was so successful that Newman was invited in the early 1970s to advise the government of Hong Kong—then dealing with a rise in heroin use after the British banned opium smoking—on how to implement their own methadone program. Newman recently wrote about his experience advising Hong Kong, and what America, once again dealing with a proliferation of opioid use disorder, can learn from it.
I spoke with Newman over the phone this week about what Hong Kong did, what New York City did, why those plans worked, and what the U.S. could be now doing differently to help folks with opioid use disorders who'd like to transition to a less potent drug. It will surprise few people following this issue that bureaucratic red tape is a large part of the problem.
Our conversation has been edited for clarity and length.
Reason: I want to hear about New York, but first, I'm curious about Hong Kong's decision to allow lay people to play a big role in methadone treatment.
Dr. Newman: It was pure pragmatism. I was Hong Kong's consultant, and I recommended the usual array of well-trained specialists, such as physicians and nurses and social workers. When I came back to Hong Kong a year after they'd started the program, they had 5,000 people in treatment and very few of those specialists. I asked them how they did that, and the Hong Kong folks, in their usual polite wonderful way, told me that my recommendations were fantastic, but they didn't have any social workers. They didn't have any nurses. But they also didn't want to leave people on the street who could be helped by methadone treatment, so they proceeded without those specially trained people.
It was never, "Ah, we don't need nurses! We don't need social workers!" They focused on where they had to go. The goal was to make treatment immediately available to everybody who wanted it. The only way to achieve that was to forego the professional staffing and go with non-professional staff. It was every bit as successful as other countries, including the U.S., which relies exclusively on well-trained specialists.
Reason: It seems we have the same shortage of specialists who want to provide medication-assisted therapy (MAT) with methadone and suboxone, or at least enough people who are qualified in the eyes of Health and Human Services to offer that treatment.
Dr. Newman: I'm actually not sure that we do. We certainly had no problems back in the early '70s recruiting physicians. We had no problem recruiting nurses and we had no problem recruiting counselors. Although, at the time, the requirements for counseling were essentially nonexistent. You didn't have to be certified. You didn't have to be accredited. You didn't need a degree. Anybody could be appointed as a counselor. But we didn't have any problem with nurses or doctors, either.
I imagine that today, if you were willing to pay the price, you could get doctors and nurses. I haven't heard of any methadone clinic anywhere in the U.S. that received approval to open but couldn't recruit the professional staff.
But in Hong Kong, they could not recruit the staff. They had a paucity of them. There were physicians who were part-timers, but they had no social workers and no nurses. And it worked out extremely well regardless. Teaching volunteers was not hard. If the order sheet called for 40 milligrams, you pulled the syringe up to 40, you squirted it into a cup, and you handed it to the patient.
For social work, they were initially subjected to all kinds of criticism by foreign visitors who came to observe their program and asked how they could just ignore the social service needs of their patients. Once again, they dealt with this criticism with enormous pragmatism. They put a sign up over every dispensing station at every clinic that said, "If you have social service needs, the nearest social service office is located at," and then they gave the address. And that was it.
Nowadays, there are more social workers available. And, again, it was not a philosophical objection to social work. They just weren't going to abandon people because they couldn't meet the requirements that I and other foreign experts said were important.
Reason: What's keeping the U.S. from scaling up treatment services? It seems like we have a weird obsession with abstinence-based treatment, we have federally imposed limits on how many MAT patients doctors can see concurrently, and neighborhoods don't want methadone clinics.
Dr. Newman: All of the above. The problem here is that there are really few, if any, advocates who are focused on the life-and-death needs of individuals who want treatment, need treatment, could benefit from treatment, but can't get it. There are patient advocates, there are program advocates, there are professional organizations representing the perspectives of care providers, but nobody is focused on the needs of people who can't get into treatment.
Two days ago, I heard a news story from Everett, Washington, which is 40 miles north of Seattle. The city is considering—despite lots of opposition—a second methadone clinic, because the only one they have right now serves 600 patients per year, and has 200 people on the waiting list. Last month, I saw articles about methadone waiting lists in California and the Carolinas.
It need not be that way! New York was able to eliminate its waiting list in 1973. 1973! It can be done if the commitment is there to do it.
Reason: Should clinics be helping more patients, or do we just need more clinics?
Dr. Newman: We need both. And we need physicians to step up. For the last 20 years, it's been possible for physicians to take a ridiculously simply eight-hour session online in order to prescribe buprenorphine, which goes by the trade name Suboxone. And yet there are very, very few physicians around the country willing to do that.

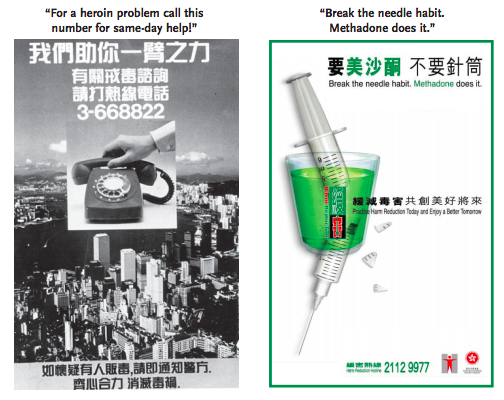
The fundamental need is for some authoritative body to say, "The current situation in the U.S. is not acceptable." And it's not just waiting lists. We should have posters in every emergency room saying, "Dependence on painkillers and heroin is a treatable condition. Ask the staff about your treatment options." That doesn't exist anywhere in the country. Hong Kong has had these posters going back 40 years. "Call the following number for an immediate referral to methadone treatment."
The commitment is lacking. In addition to more physicians and more clinics, we have these federally mandated capacity limits telling doctors they can only treat so many MAT patients. Who ever heard of capacity limits in any other field of medicine? Can you imagine a prenatal clinic being bound by a federal mandate that says, "You cannot have more than X number of pregnant women that you care for"? Can you imagine a prenatal clinic turning pregnant women away and saying, "Come back in 10 or 12 months?" Only in this field do we tolerate these regulations.
A couple of years ago, Baltimore offered a pilot program in which people on their waiting list could receive methadone without any other services. It's very much like what Hong Kong did 40 years ago. And they found the results were absolutely fine. Patients who were receiving methadone while awaiting admission to the full program did every bit as well as patients receiving comprehensive treatment.
And the costs! The incremental costs to make just the medicine available was $3.50 per patient per week.
Reason: Even if the cost were $30 per patient per week, methadone on demand would still be exponentially cheaper than the abstinence-based, in-patient treatment programs that seem to receive so much funding.
Dr. Newman: It would indeed. And it would allow a substantial number of waiting list patients, many thousands of whom are willing to pay $100 a week out of pocket—essentially the full cost of comprehensive methadone treatment—to get the drugs they want and need while waiting for a spot to open. It would certainly be better than telling them, "Come back later. In the meantime, we hope a friend of yours is ready to administer naloxone."
Reason: We've lost our sense of urgency.
Dr. Newman: We sure have! We have all these people begging for treatment even though they know the federal government demands—demands!—that new patients attend a clinic daily for the first nine months and that they pee in a cup under direct supervision. One of the most amazing things to me, even after 40 years in this field, is the motivation that people have to get treated. You don't see it in any other field of medicine. And there are so many people applying for that kind of treatment, and they're being ignored. It's unthinkable.
Reason: One of things you bring up in the paper that seems like a huge obstacle here is that Hong Kong said, "Let's help the most people as fast as possible, and not let the perfect be the enemy of the good." I follow conversations among doctors who treat substance use disorders, and they seem to be concerned that if they don't do this in the best possible way, in the most comprehensive way, they'll lose ground. That if it's not perfect, they won't get a second bite at the apple. Does that strike you as new? Because your experience in New York in the 1970s was very different.
Dr. Newman: Look, it was just as oddball then as people seem to think it is now. The reason we could proceed with the good in New York—rather than wait for the perfect system—was because the guy who was the health czar of New York City was 37 years old and had no medical training. Gordon Chase was appointed by Mayor Lindsey to be basically in charge of all health and hospital services in New York City. He wasn't smart enough or educated enough to know that you're supposed to have comprehensive services, that you're supposed to go slow, that you're supposed to take your time to train people. He didn't know any of that.
He assigned me the job of overseeing an unprecedented expansion of methadone treatment. And I didn't have any experience in the field either! Basically, I agreed with the guy I worked for. For us, it was a question of compared to what? I never had a reason to doubt that the good would indeed be very good, and that it would at worst be better than doing nothing.
Reason: So what explains the cautiousness of people who know how bad this problem is?
Newman: When we talk about resistance in the health care field, we're talking about asking folks to endorse an approach that is different from theirs and that is also much less costly than theirs. And there is concern, which I can appreciate, that if it's shown you can provide reasonably good treatment without all the expenses associated with a comprehensive program, that funders will then say, "Well, if this works well enough, why should we pay for all these social workers? All these comprehensive programs?"
That's a universal fear. I saw it when I was consulting in Germany, and even early on in Hong Kong. But it's a fear that's never been born out. In Hong Kong, as in New York, drug-free residential programs, as expensive as they were, continued to be supported and expanded, just as they were before large-scale methadone expansion. People think it's "My way, or the highway," but that's wrong.
I don't want to sound critical. All of these people we're talking about are dedicated to providing the best—not just good—but the best care for the patients who have come to them, for whom they are responsible. They don't want to compromise the quality of care for the people they're treating. And that's great for the people who are already in treatment!
But again, we're talking about the people who are not in treatment and who can't get treatment because there aren't enough spots in perfect programs.
I'm realistic enough to know that financial self-interest may play a role, as well as therapeutic authority and power, but I think there's a much more generous and accurate explanation, which is that these are providers who simply refuse to compromise on the comprehensive care they provide. But again, those fears have never been realized. Even when studies demonstrate that you don't need comprehensive services to save a lot of lives, we continue to support the best care at a substantial price.
And that's fine, so long as somebody cares for the people who are getting no treatment at all. There are a lot of them out there, they are dying, and we need to give a damn about them.


Show Comments (99)