Cancer Death Rate Continues to Fall: Incidence Declines for Men and Remains Steady for Women
Good news: Cancer mortality rate has dropped from its peak of 215.1 (per 100,000 population) in 1991 to 166.4 in 2012.
CORRECTION: The data in this item are correct, but out of date. I erroneously reported these as being the latest figures, but actually the American Cancer Society has issued Cancer Statistics 2017. I have now reported as a correction to this post the new data here. The good news is that trends in both cancer death rates and incidence are even better in 2017. I hope that readers were not unduly confused by my error.
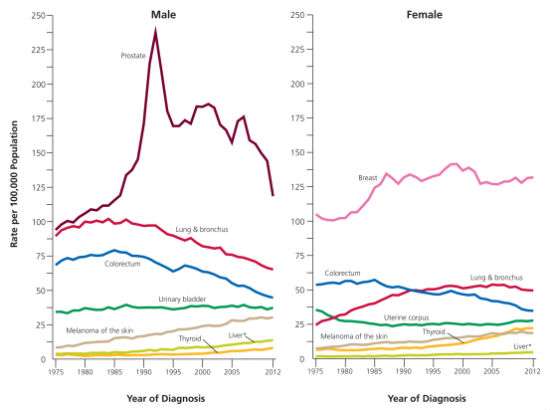
The cancer death rate has dropped by 23 percent since 1991, translating to more than 1.7 million deaths averted through 2012, according the latest Cancer Statistics 2016 report from the American Cancer Society (ACS). Cancer incidence - percent of folks who get cancer each year - has also fallen since the early 1990s. The falling incidence trend continues in the latest report for men, declining by 3.1 percent year between 2009 and 2012. However, the cancer incidence rate remained steady for women over that period. A lot the falling rate of cancer incidence can be chalked up to less lung cancer as fewer people smoke and more colonoscopies which prevent colorectal cancer. In addition, the report notes that the recent rapid decline in prostate cancer diagnoses accounts for about one-half of the total incidence decrease in men. The reduction in prostate cancer diagnosis is largely the result new guidelines from the U.S. Preventive Services Task Force against routine screening with the PSA test because of growing concerns about high rates of overdiagnosis. It is worth noting that that contrary to the USPST's blanket recommendation, the American Cancer Society urges men to talk with their physicians about the risks and benefits and decide for themselves whether they want the screening test.
The new ACS also notes that thyroid cancer rates appear to be increasing largely because the advent of more sensitive screening tests that identify lots of cancers in people over age 50 that are not clinically relevant; about 50 percent in women and 40 percent in men.
The report futher notes:
The lifetime probability of being diagnosed with an invasive cancer is higher for men (42%) than for women (38%). Reasons for increased susceptibility in men are not well understood, but to some extent reflect differences in environmental exposures, endogenous hormones, and probably complex interactions between these influences. Adult height, which is determined by genetics and childhood nutrition, is positively associated with cancer incidence and death in both men and women, and has been estimated to account for one-third of the sex differences in cancer risk.
Being male and standing at 6 feet 5 inches, I'm at higher risk, but the mortality trends give me some scope for optimism. After all, at a conference in 2015, Dr. D. Gary Gilliland, president and director of Fred Hutchinson Cancer Research Center, declared, "It's actually plausible that in 10 years we'll have curative therapies for most if not all human cancers."
With regard to mortality trends, the ACS reports:
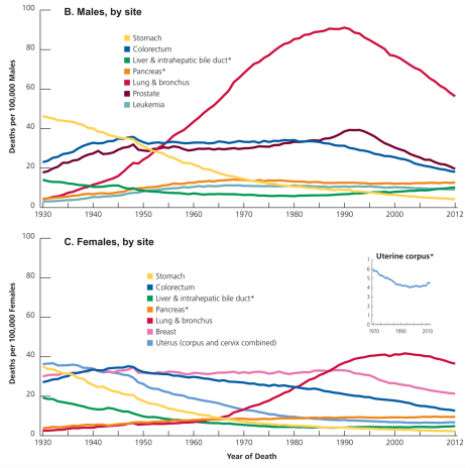
The overall cancer death rate rose during most of the 20th century, largely driven by rapid increases in lung cancer deaths among men as a consequence of the tobacco epidemic. Steady reductions in smoking, as well as advances in cancer prevention, early detection, and treatment, have resulted in a 23% drop in the cancer death rate, from a peak of 215.1 (per 100,000 population) in 1991 to 166.4 in 2012. The decline, which is larger in men (28% since 1990) than in women (19% since 1991), translates into the avoidance of approximately 1,711,300 cancer deaths (1,199,200 in men and 512,100 in women) that would have occurred if peak rates had persisted.
One more takeaway: There is no rising cancer epidemic; much less one that can be attributed to modern technologies like cell phones, genetically modified crops and trace exposures to synthetic chemicals.


Show Comments (9)