New CDC Estimates Suggest COVID-19 Is Deadlier Than the Agency Previously Thought
The increase in the estimated infection fatality rate is especially large for the oldest age group.
The latest estimates from the Centers for Disease Control and Prevention (CDC) suggest COVID-19 is deadlier than the CDC previously thought, especially among older Americans. According to the "best estimate" in the most recent version of the CDC's COVID-19 Pandemic Planning Scenarios, 9 percent of people 65 or older who are infected by the COVID-19 virus die from the disease. The estimated infection fatality rates (IFRs) for other age groups are much lower but still generally higher than the numbers the CDC was using prior to March 19.
The estimated IFR is 0.002 percent for people 17 or younger, 0.05 percent for 18-to-49-year-olds, and 0.6 percent for 50-to-64-year-olds. The CDC's prior estimates used somewhat different age groups, which makes direct comparisons tricky. But the estimated IFR for the oldest age group has risen dramatically, from 5.4 percent for 70+ to 9 percent for 65+.
The new estimates are also higher for the second-oldest group (0.6 percent for 50-to-64-year-olds now vs. 0.5 percent for 50-to-69-year-olds previously) and the second-youngest group (0.05 percent for 18-to-49-year-olds vs. 0.02 percent for 20-to-49-year-olds). The new estimate for the youngest age group is lower (0.002 percent for 17 or younger vs. 0.003 percent for 19 or younger), but that may reflect the lower cutoff.
The CDC's earlier estimates were based on a July 2020 PLOS Medicine study that used data from Hubei, China, and six regions of Europe. The Chinese numbers were reported in January and February 2020, while the European numbers were reported in March and April 2020. The CDC's new estimates are based on a systematic review and meta-analysis published by the European Journal of Epidemiology in December. The meta-analysis was based on 27 studies covering 34 locations, including a dozen each in the United States and Europe.
The CDC's new numbers do not include an overall IFR for the United States, which a July update estimated was about 0.65 percent. That estimate presumably would be higher now.
How much higher? We can get a rough idea from the CDC's estimates of how many people have been infected in each state (except for North and South Dakota). Those estimates are based on antibody testing of blood drawn for diagnostic tests unrelated to COVID-19 from patients across the country. Although the patients in those samples are not necessarily representative of the general population, the prevalence numbers, combined with contemporaneous COVID-19 death counts, can be used to roughly estimate IFRs.
Dividing the U.S. death toll as of February 28 by the total estimated number of infections on that date (around 65 million) suggests a nationwide IFR in the neighborhood of 0.8 percent. But that average conceals a great deal of interstate variation.
As of February 28, for example, the CDC estimated that 401,000 Connecticut residents had been infected by the coronavirus. The state's death toll at that point suggests that Connecticut's IFR was about 1.9 percent. In Utah, by contrast, the CDC estimated there were 874,000 infections at the end of February, which suggests an IFR of about 0.2 percent. The implied IFR is about 0.6 percent for Texas and California, about 0.8 percent for Florida, about 0.9 percent for Pennsylvania, and about 1.8 percent for New York.
While the CDC's prevalence estimates may be imprecise, the wide range of implied IFRs corresponds to a wide range of case fatality rates (CFRs)—deaths as a share of confirmed infections. The current CFR is 2.5 percent in Connecticut, for example, compared to less than 0.6 percent in Utah. Patients clearly face better odds in some states than others.
Given the stark differences in COVID-19 risk between age groups, age demographics may explain some of this variation. Other possible factors include the prevalence of preexisting health conditions, the capacity and quality of local health care systems, and population density, which not only affects how fast and far the virus spreads but also may affect viral doses and therefore the severity of infections. And assuming that medical treatment of COVID-19 improved over the course of the pandemic, patients in states that had relatively late outbreaks may have fared better as a result.
[This post has been revised to include a paragraph about case fatality rates.]
Editor's Note: As of February 29, 2024, commenting privileges on reason.com posts are limited to Reason Plus subscribers. Past commenters are grandfathered in for a temporary period. Subscribe here to preserve your ability to comment. Your Reason Plus subscription also gives you an ad-free version of reason.com, along with full access to the digital edition and archives of Reason magazine. We request that comments be civil and on-topic. We do not moderate or assume any responsibility for comments, which are owned by the readers who post them. Comments do not represent the views of reason.com or Reason Foundation. We reserve the right to delete any comment and ban commenters for any reason at any time. Comments may only be edited within 5 minutes of posting. Report abuses.
Please to post comments


BE FRIGHTENED PEOPLE! GET YOUR PASSPORT NOW!
ok https://profitjam-review.medium.com/endgame-review-james-fawcett-et-al-endgame-oto-endgame-upsell-5000-bonuses-62fbc0c3426f
My last pay check was $8750 just ecom working 12 hours for every week. My neighbor dcs have found the estimation of $15k for a long time and she works around 20 hours for seven days. I can not trust how direct it was once I tried it information.. Visit Here
Everybody can earn 50 dollars Daily.you can earn more than you think by working online from home. I have been doing this job for like a few weeks and my last week payment was exactly 2537 dollars...........USA PART TIME JOB.
My last pay check was 8750 dollars just ecom working 12 hours for every week. My neighbor have found the estimation of 15000 dollars for a long time and she works around 20 hours for seven days. I can not trust how direct it was once I tried it information...........USA PART TIME JOB.
LIFE CHANGING OPPORTUNITY BE an Internet HOME-BASED real Earner.I am just working on facebook BHY only 3 to 4 hours a Day and earning £47786 a month easily, that is handsome earning to meet my extra expenses and that is really life changing opportunity. Let me give you a little insight into what I do..... Visit Here
[ PART TIME JOB FOR USA ] Making money online more than 15$ just by doing simple works from home. I have received $18376 last month. Its an easy and simpleBTTY job to do and its earnings are much better than regular office job and even a little child can do this and earns money. Everybody must try this job by just use the info
on this page…. Visit Here
https://flipplyreview.medium.com/magnum-oto-magnum-upsell-magnum-bonuses-magnum-store-builder-review-adcd643f5dd1
Also, is Sullum Reason's Thomas Friedman?
Cleaning company in Jazan
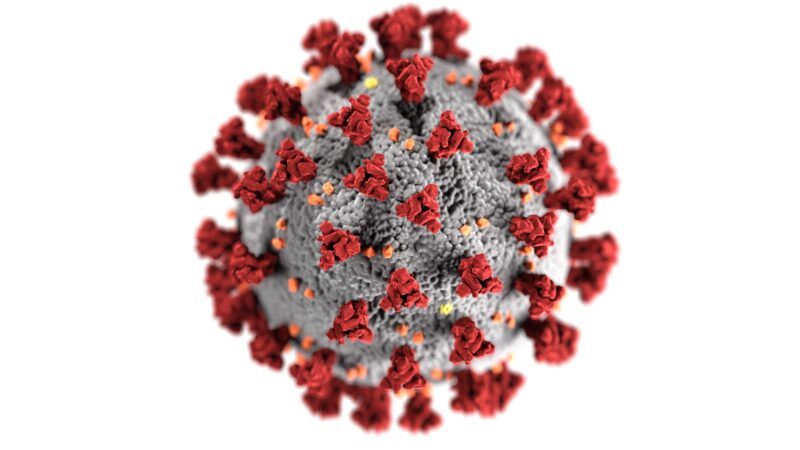
That rendering of Covid looks fuzzy and soft. How can you fear something that friendly looking?
How to explain such a stark difference in IFR between NY and UT: 1.8% vs 0.2%?
In addition to the reasons given here, I think that a big part of the answer is political divisiveness: libs infected their vulnerable wards for political gain. There was so much hate, and the stakes were so high to exacerbate the crisis, that it was inevitable. Not saying that people did it intentionally. But it wasn't entirely unconscious either.
They did do it intentionally. That’s the sick part.
E.G., Cuomo chose to take nursing home campaign cash to give them a liability waiver for the virus, and he chose to put Covid patients in nursing homes rather than the facilities Trump provided so he didn't have to thank Trump. Other D governors did the same.
If government wasn't so involved in nursing homes, they'd be safer, better and less expensive. Free markets deliver, but not to politicians.
You mean it's going to kill grandma more than Cuomo already did?
Regardless of the exact numbers, it's beyond clear that opening up doesn't result in a huge explosion of cases and overwhelming of the medical system. All restrictions should be lifted and voluntary measures used instead. Consent, you know!
Quoting the CDC is ridiculous now, they are in thrall to the hard left of this administration.
Fuck you and your increase in the chocolate ration, CDC. The disease has been on these shores for a year, and you're getting these kinds of fluctuations in the death rate? Yeah, sure.
The new numbers aren't fluctuations in the death rate. The IFR numbers now are quite close to the numbers from one year ago from NOT the CDC.
The bogus numbers in the interim are a result of political/journalistic pressure overriding any interest in truth.
Both D's and R's - and Sullum for that matter - have had a desire - for different reasons/narratives - to increase the IFR denominator. Hey presto what is sold turns into what is
In my county we know for certain that a 40-year old man in a motorcycle accident that died from his injuries at the hospital and whose corpse tested positive for COVID was declared a COVID death. Two broken legs and skull fractures could not have played a major part. I mean, he felt well enough to get on a bike, didn't he?
the coroner was forced to reclassify the death as a motor vehicle accident, so the hospital missed out on the $16,000 federal money.
Makes one wonder how many of the COVID deaths were mostly caused by COVID.
Most of them.
I have signed dozens of death certificates that have Covid listed as a cause of death. One or two of them was accurate. Lots of people are dying with Covid, not necessarily from Covid.
Which is not actually relevant. What is relevant is the total number of excess deaths. Those are the people who are - you know - DEAD now. There is no miscounting of dead people. No hiding them.
There is some possible error in determining what is 'excess' - but mostly that is Stats101 stuff. Not some actual dispute about what is. There are about 550,000 - 650,000 excess deaths. Of which about 100,000 are put into a non-Covid category - eg 15k excess cerebrovascular (stroke), 4.8k cancer, etc.
Which leaves a huge remainder there - which you want to ignore because you want to pretend Covid doesn't really exist. And bluntly - many of those other specifically mentioned non-covid causes of excess deaths - notably vascular, respiratory, and Alzheimers - are more likely to be covid-related-but-undiagnosed than they are to be either lockdown related or 'seasonally fluctuating outside excess bounds'.
Stay scared, my friends.
100K lock down induced deaths.
Unfortunately all info from now until forever from CDC is going to be bogus noise. Since they chose not to do much seroprevalence/antibody testing to track actual exposure to the virus as it spread, there is no solid baseline for estimated infections. Can't measure an IFR without a valid denominator.
And can't meaningfully measure antibodies from now because its impossible to know whether those antibodies now result from exposure to the virus or the vaccine.
Even if CDC had a highly 'libertarian' approach to public health of - oh - let them eat zinc; it is unforgivable that they failed to even produce the data that lets us know what actually happened. There are certainly some public health agencies in the world that did a reasonable job here. CDC ain't one of them. And a public health agency that doesn't even know how to deal with a pandemic is pretty fucking useless.
Science denier!
For many people this is their first intense exposure to the many uncertainties involved in epidemiology and such things as determining a primary cause of death. Hence there has been a lot of mistrust and animosity generated toward public health agencies because of the restrictive measures imposed.
In a sense we all were infected with this disease and all suffered because of it. That has not happened before in our lives. We did not question the number of flu cases a few years ago or the number of deaths from it although it is subject to the same uncertainties.
The "restrictive measures imposed" constituted the worst policy decision - outside of war related calamities - in a thousand years. Focused protection should have always been the goal. The age stratification of death rates has been known (and stable) since April/May of last year. Quarantining the healthy was monstrously stupid creating an excess death shadow that will live with us for a decade or so.
In a sense we all were infected with this disease and all suffered because of it. That has not happened before in our lives.
Unless you count the previous coronavirus pandemics, flu pandemics, measles, chickenpox, HPV, CMV, etc., etc., etc. And then it happens a lot. But, in a sense, you're right; nothing like this has happened to anyone born in the 21st Century.
Except CDC has also estimated that 4.6 times more Americans were infected with covid (than have tested positive for covid).
https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/burden.html
Since 9.4% have tested positive for covid, the CDC estimates 43% of Americans have been infected with covid.
The good news is that virtually everyone previously infected with covid remains immune.
Old people die!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!
Alert the Media - This is BIG news.... NOT.
Every-single complication known to man is heavier in the old category.
keto cookbook free download pdf
And the Democrats' response = "But, Trump!!!"
Well, your risk of dying if you get COVID can't suddenly shoot up from 0.6% to 9% when you turn 65. So either those numbers are suspect, or the "65 and over" group needs to be broken down into sub-groups. What is the risk for people 65-74? 75-84? etc.
Bullshit. More speculation, data contortions and fear porn.
From using a high cycle PCR test to classifying the mere presence of COVID in a deceased as a COVID death, we'll never know the actual impact of COVID on the population.
There is a difference between being over 65 and dying because of COVID, as opposed to dying while testing positive for COVID. The statistics are inflated because many of the latter are lumped together with the former.
The IFR has stayed pretty constant at 0.6% since it was first made obvious from cruise ship statistics over a year ago.
There are about 300 million people in the USA. Hardly anyone lives past 100 years of age, so to make the math easy say 3 million people die in a normal year. If 20% of the nation caught COVID-19, about 600,000 people would have died with COVID-19 in the past year. The latest total per Google is 554K.
And if 20% of 300 million people caught it (60 million) and 0.6% died from it, that would be 360K deaths caused by COVID-19 (not just WITH COVID-19).
DING DING DING DING DING
I've been saying this since the start. We see over and over that the bug gets to roughly 20% prevalence and then falls off a cliff. If 20% of your population gets the bug, you'd expect 20% of your deaths to have it in their system, especially with our ridiculous over-sensitive tests.
That's 600,000.
This simple system can turn any new bug into 600k deaths.
Covid-19 has certainly affected every aspect of human life
"estimates are based on antibody testing of blood drawn for diagnostic tests unrelated to COVID-19 from patients across the country. Although the patients in those samples are not necessarily representative of the general population, the prevalence numbers, combined with contemporaneous COVID-19 death counts, can be used to roughly estimate IFRs."
If by "roughly estimate" you mean badly estimate, maybe. People in the age groups <49 years old are not commonly getting diagnostic tests requiring a blood draw, so the IFR is likely being overstated for them by severely undercounting those that were asymptomatic or had minor symptoms.
Agree. Even if they correct for age group bias, there is no way to correct for the cohort that has diagnostic blood tests performed. There is no way to perform a correction that makes the stats in the group representative of the whole population because of the very reasons they are getting blood tests.
The US is rapidly becoming a world leader in vaccination for Covid. People are also opening things up more whatever the government says. Today is Easter. Family and friends will get together as they should.
Quibbling about death rates is not important now. We all know this is a serious disease which can result in significant morbidity and mortality. The focus should be on getting jabs and getting our world back together.
My mother was able to travel to spend the final days of Passover with 14 family members. She is a great grandmother many times over. Some came from as far away as Israel. It is good to see our lives beginning to come back.
Happy Easter and enjoy the day.
One big problem with the analysis when using US data is the assumption that the antibody prevalence indicates how many caught the disease. When you go to the CDC's dashboard, you see a number of states where the prevalence has been gradually decreasing. This could be a difference in sampling, but I think at least part of it is that antibodies decrease below detectable levels over time for some nontrivial portion of the population. The result is that you'll believe fewer and fewer people have been infected, which drives up the IFR.
What’s for dinner tonight? Hope you can all get together. We don’t celebrate Easter but Passover Seder was not to be beat. We are getting together with a few people later because it is my daughters birthday. Nothing fancy. We do have some bottles of wine left so gonna open those. Carry out Chinese or something.
I guess I am getting kinda burned out on all of that arguing. I see things starting to change and turn around. Last year at this time was a nightmare. Now it is much less of a nightmare. It will only improve from here out.
So there are some things to be thankful for.
And good to hear you are all recovered and back to health.