Even in Health Care, Immigrants Do Jobs Americans Won't
If we want to solve the doctor shortage, we should import more foreign physicians.


The debate over American health care tends to focus on how we pay for services, rather than why we pay so much more than any other developed country. In a new working paper, Jeffrey S. Flier and Jared M. Rhoads of the Mercatus Institute suggest that we could lower costs by allowing more people to practice medicine.
In a comparison of 11 industrialized nations, they write, the U.S. has the second lowest number of physicians per capita: "2.5 physicians per 1,000 population, compared to a mean of 3.1 for the group and high of 4.2 for Norway." The Association of American Medical Colleges anticipates a shortage of 40,800 to 104,900 physicians by 2030, particularly in the fields of pediatrics, primary care, family medicine, and internal medicine. (Not coincidentally, these are four of the lowest-paying medical specialties.)
The association wants to address that shortage by securing more federal funding for physician training, but with no concessions on tuition, which averages $55,000 per year in the United States. Flier and Rhoads have some other suggestions: expanding the number of accredited U.S. medical schools, shortening the length of medical school, granting more independence to nurse practitioners and physicians assistants, and reforming state licensing boards so that medical doctors can no longer use their clout to suppress competition.
We could also, they add, make it easier for foreign-born, foreign-trained doctors to migrate to and practice in the U.S. Indeed, there are roughly 60,000 foreign medical doctors already living in the U.S. who aren't licensed to practice.
Foreign-born medical doctors who trained outside the U.S. already play a crucial role in providing care in America. These physicians "are substantially more likely to practice in rural and poorer communities and are overrepresented in primary care specialties, including family medicine and pediatrics," write Flier and Rhoads. A 2015 study found that international medical graduates (a group that includes Americans who train outside the U.S. and foreign citizens who train outside the U.S.) are filling a crucial care gap:
IMGs are more likely to practice in specialties in which a physician shortage would otherwise go unfilled. For example, a higher proportion of IMGs than other graduates serve socioeconomically disadvantaged populations across the United States. They also tend to fill the gaps in workforce demands in rural areas depending on the particular state. One study reported that 19.3% of IMGs, compared with 10.4% of osteopathic physicians, are practicing in rural areas. An ambulatory care survey published in 2009 found that most office-based IMG primary care physicians are in areas with physician shortages where Medicare and Medicaid patients are overrepresented. Compared with US medical graduates, a higher percentage of IMGs are also in solo practice. Overall, IMGs have been taking up opportunities to practice within patient populations that are facing difficulties caused by uneven distribution of the physician workforce.
It's possible that foreign doctors have lower debt loads and can thus pursue lower-paying specialties, or, because the American residency system prefers American born-and-trained physicians, that IMGs fill less desirable roles in order to practice in the U.S. at all. Either way, they're often willing to go to areas many American-trained physicians are not. Like Nebraska.
Every year, the National Residency Match Program publishes data showing what types of doctors matched to what kind of medical residency in each state (a medical residency of at least a year is required in order to receive a medical license in the U.S.). Here's what the numbers look like for Nebraska, which had a total of 93 open positions for family medicine and internal medicine in 2017:
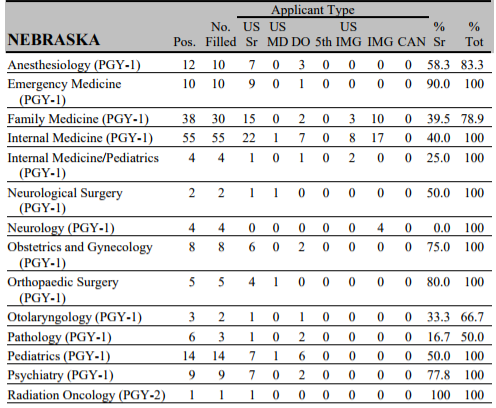
Across the top of that chart are the various applicant types. "US sr" are fourth-year medical students attending allopathic medical schools in the U.S.; they will be M.D.s upon graduation, and 94 percent of them will "match"—as in, be selected for—a U.S. residency. Further to the right is "IMG," non-U.S. citizens who attended international medical schools; they land the fewest residency slots each year, with roughly 50 percent of applicants matching. In Nebraska, non-U.S. citizens who attended foreign medical schools filled 33 percent of the year-one primary care and internal medicine residency slots, and 100 percent of the neurology positions. In California, non-U.S. citizens who trained overseas filled only 10 percent of the internal medicine and family medicine slots.
More physicians want to live and work in California than in Nebraska, and American residency programs tend to favor U.S. citizens over non-citizens. Even in medicine, immigrants end up doing the jobs Americans won't.
What's more, foreign medical school grads are willing to do this work even though the U.S. licensure system penalizes physicians who train abroad by requiring them to do a residency regardless of whether they're already licensed to practice in their home country. This means not only that the U.S. can only import as many physicians as there are low-tier residency slots, but also that we spend Medicare money retraining foreign-born physicians without regard for their level of competence.
Canada also faces a doctor shortage, and it has turned to the international market to fill it. But rather than requiring every foreign medical school graduate to undergo retraining, Flier and Rhoads write, immigrants "may bypass postgraduate training requirements [in Canada] if he or she did residency training in Australia, Hong Kong, Ireland, New Zealand, Singapore, South Africa, Switzerland, the United Kingdom, or the United States." Most foreign-born-and-trained doctors who come to the U.S. are from India, the Philippines, Mexico, Pakistan, and the Dominican Republic, and there might be legitimate questions about the quality of training in those places. But that's an assumption we should interrogate, and even if it's accurate, it doesn't preclude the creation and administration of some kind of comprehensive equivalency exam that could assess whether their skills were transferable. Regardless of how we handle the question of reciprocity, importing more foreign physicians could save money and lives.


Show Comments (38)