Five Years and $500 Million Later, USDA Admits That 'Food Deserts' Don't Matter
You can lead people to Whole Foods, but you can't make them buy organic kale.


For several years, so-called "food deserts"—low-income neighborhoods devoid of nutritious food options—were an oft-cited culprit for America's high obesity levels. Everyone from state senators to Michelle Obama had ideas about how to fix the issue, from launching new farmer's markets in these neighborhoods to state grant programs designed to entice more fruit-and-veggie offerings to bans on new fast-food restaurants opening in these areas. The kicker was a multi-million dollar federal initiative, spearheaded by the First Lady, to promote farmer's markets and attract more grocery-store chains to food-desert neighborhoods.
"Since 2011, the Federal Government has spent almost $500 million to improve food store access in neighborhoods lacking large, well-stocked grocery stores," according to the U.S. Department of Agriculture (USDA). "States and local governments have also launched programs to attract supermarkets or improve existing stores in underserved areas. For example, the Pennsylvania Fresh Food Initiative has provided $30 million of public funds (matched with $117 million of private investment) to help address limited store access in underserved urban and rural areas throughout Pennsylvania."
The theory was simple: poor people simply lacked easy access to healthy food options. If you put fruits, vegetables, and whole grains in front of them, they would soon be singing the praises of Michael Pollan, too. And voila: no more obesity epidemic in these neighborhoods.
But of course things didn't work out that way. As many business owners in these neighborhoods and other food-desert skeptics have pointed out, the problem wasn't that they simply hadn't thought to offer more wholesome items. The problem was that these items just didn't sell. You can lead human beings to Whole Foods, but you can't make them buy organic kale there.
The USDA just admitted as much, with a new report on food deserts published in its magazine, Amber Waves. Highlights from the article note that proximity to supermarkets "has a limited impact on food choices" and "household and neighborhood resources, education, and taste preferences may be more important determinants of food choice than store proximity."
While limited early research "found a positive correlation between access to a supermarket (or other stores selling a wide variety of healthful food) and diet quality," these studies generally only measured food purchases for a short time period and often failed to "consider the fact that most households have access to a vehicle and are able to travel beyond the local food environment to shop for groceries." More recent and robust data "show that the effect of food store access on dietary quality may be limited."
Using data from several national food studies, the USDA determined that both low- and higher-income households tend to shop at supermarkets. Overall, 90 percent of households in a 2012-2013 study shopped for groceries at "a supermarket or supercenter." The figure was nearly identical for households that participate in USDA's Supplemental Nutrition Assistance Program (SNAP)—what used to be known as food stamps—or the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), and for households deemed as "food-insecure."
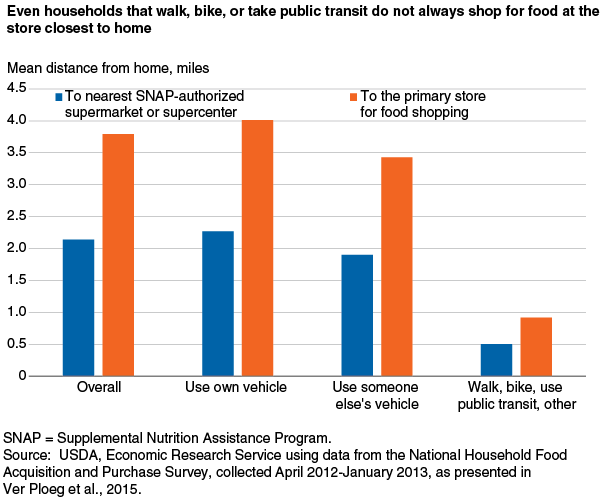
Both low and higher-income households also tend to travel to shop, often bypassing the nearest market when getting groceries. "This behavior was consistent across transportations modes; even those who walk, bike, or take public transit traveled, on average, farther than the distance to the nearest supermarket to do their primary food shopping," the USDA states. This suggests "that most U.S. households are not limited by the food stores in their own neighborhoods."
In low-income neighborhoods defined as food deserts, "limited food store access showed a modest negative effect on the nutritional quality of consumers' diets," with consumers in these neighborhoods purchasing 4.3 percent less fruit, 2.4 percent less vegetables, and 10.4 percent less low-fat milk products than consumers not living in such areas." (Why the government persists in defining low-fat milk as the healthiest milk option is a mystery.) Customers in these areas also bought more diet drinks, more red meat, more poultry, and more fish.
The USDA notes that another recent study found SNAP beneficiaries "were more sensitive to price than to food store access. Participants with very difficult access purchased smaller amounts of perishable foods than shoppers with easy access. However, the prices of different food groups were more important determinants of purchase decisions than was access. When price and demographic factors were accounted for, the effects of food access were negligible." When considering 13 food groups, "price increases led to statistically significant declines in purchases by SNAP households for all 13." But difficulty in accessing an item was associated with fewer purchases of only one food group (noncanned fruits and vegetables).
Research looking at specific low-income neighborhoods and the effect of new grocers opening found no association between shopping at the new store and dietary improvements and found slightly decreased consumption of fruit and vegetables. A 2014 study of two neighborhoods in Philadelphia found the opening of a new supermarket improved "residents' perceptions of food accessibility in the neighborhood" but did not lead to increased consumption of fruits and vegetables.


Show Comments (89)