Death Rate for Middle Aged U.S. Whites Anomalously Rising
Drugs, suicide, and liver disease responsible for 500,000 extra deaths since 1999.

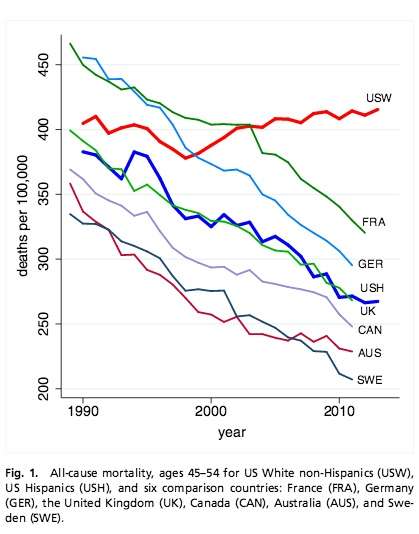
In a disturbing new study by Princeton University researchers Anne Case and Angus Deaton finds that the death rates for middle-aged American white people - ages 45 to 54 years - has been rising since 1999. (Deaton is this year's Nobel Economics Laureate.) The rise in white midlife death rates is found entirely among those Americans with a high school degree or less. The 2013 mortality rates for midlife whites with high school degree or less is 736 per 100,000; for those with some college education it is 288 per 100,000; for whites with a B.A. or higher their death rate stands at 178 per 100,000. In other words, whites who have only a high school degree or less are four times more likely to die between ages 45 and 54 than are college-educated whites. For comparison, the overall death rate for midlife Black non-Hispanics and Hispanics is 582 and 270 per 100,000 respectively.
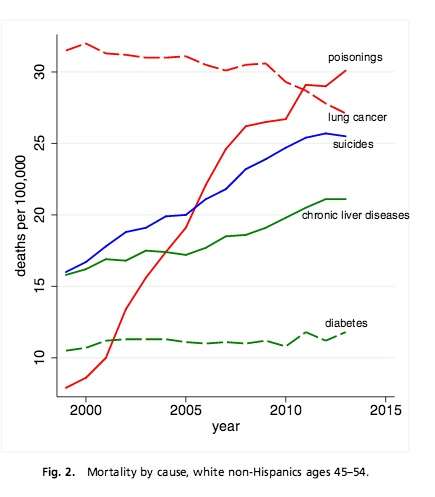
Nearly two-thirds of the increase in the white midlife death rate is the result of drug overdosing. Most of the rest is attributed to increased suicide and chronic liver diseases like alcoholic cirrhosis. The death rate in 2013 for midlife whites with a high school education or less from drug poisoning, suicide, and cirrhosis is 58, 39, and 39 per 100,000 respectively. The comparable rates for college-educated whites are 8, 16, and 7 per 100,000 respectively.
As might be expected, the rising death rate is concomitant with worsening rates of disease and disability among white midlifers.
As the Proceedings of the National Academy of Sciences explains the significance of the findings:
Midlife increases in suicides and drug poisonings have been previously noted. However, that these upward trends were persistent and large enough to drive up all-cause midlife mortality has, to our knowledge, been overlooked. If the white mortality rate for ages 45?54 had held at their 1998 value, 96,000 deaths would have been avoided from 1999–2013, 7,000 in 2013 alone. If it had continued to decline at its previous (1979?1998) rate, half a million deaths would have been avoided in the period 1999?2013, comparable to lives lost in the US AIDS epidemic through mid-2015. Concurrent declines in self-reported health, mental health, and ability to work, increased reports of pain, and deteriorating measures of liver function all point to increasing midlife distress.
Despite this setback, U.S. average life expectancy of 78.8 years has continued to rise and has never been higher.


Show Comments (60)