Why Americans Can't Have Over-the-Counter Birth Control Pills
Those with standing to challenge the pill's prescription status also gain from keeping it that way.

In many parts of the world, a person can walk into a drugstore and—without physician oversight or interference—buy a pack of birth control pills over-the-counter. Perhaps several packs.
Not so in America, where the Food and Drug Administration (FDA) has been considering making oral contraceptives available over-the-counter (OTC) for more than twenty years.
"Plan B," an emergency contraceptive, became available OTC last year. That one-step pill is simply a more potent dose of the same hormones that make up regular birth control pills. There's no good medical justification for the differentiation. Yet in America, regular birth control pills remain stubbornly behind the pharmacy counter and behind the times.
A study published in the journal Contraception recently looked at birth control access in 147 countries. It found oral contraceptives were informally available or legally available without a prescription or screening in 62 percent, while legally available without a prescription but with a screening in 8 percent. They required a prescription in only about one-third of the countries, including Canada and the United States.
In December 2012, the American College of Obstetricians and Gynecologists (ACOG) officially recommended that birth control pills be converted to OTC status in America. In its committee opinion, ACOG studiously decimated the most common objections to making oral and other hormonal contraceptives available OTC. To those concerned OTC birth control pills would prevent women from choosing more effective or longer-lasting options, such as the intrauterine device (IUD), ACOG retorted that "efforts to improve use of long-acting methods of contraception should not preclude efforts to increase access to other methods."
Side effects and safety concerns? The pill is remarkably safe. It's changed little in the past fifty-some years (except to get somewhat safer to due lower estrogen content), and been tested extensively. Plenty of OTC drugs carry some risk: gastrointestinal bleeding for non-steroidal anti-inflammatory drugs like aspirin, liver damage for acetaminophen (Tylenol), and overdose for both. You can't overdose on birth control pills, and you're very unlikely to experience other serious adverse effects.
Scaremongering over the pill tends to focus on it ratcheting up blood clot risk, but this increased risk is actually very small (even for women on the relatively riskier later-generation pills such as Yaz). About 10 per 10,000 women on oral contraceptives will get a blood clot—a risk about half as high as that associated with pregnancy.
There are some conditions which make taking the pill ill-advised but, as ACOG notes, women are capable of self-screening for liabilities. In a 2006 study comparing women's self-assessment of contraindications with medical assessment, 392 of 399 participants and healthcare providers came to the same conclusions on pill eligibility criteria.
Similarly, women could read up on different types of oral contraceptives to decide which one is best for them. It's not as if prescribing these pills is a particularly precise science anyway. In the 12 years I was on the pill, I was prescribed at least ten different brands. All of them prevented pregnancy. None of them came without various problems.
A doctor's prescription is far from a guarantee for the right match, and sometimes more likely to lead to the wrong one, as doctors often push newer and pricier, but not necessarily better, brand-name pills. In any case, a woman who finds a particular pill unpleasant is either stuck with it for 12 months or faces more doctors visits and bills.
With OTC birth control pills, women would still be free to seek medical advice about their options but removed from the burden and cost of having to. "A rational person isn't going to select some birth control pills willy nilly," says Dr. Jeffrey Singer, an Arizona-based surgeon and adjunct scholar at the Cato Institute.
The point is presenting women with wide options when it comes to learning about, selecting, and accessing contraceptive choices. A woman with good health insurance and easy access to care could very well see a doctor for pill recommendations. But an undocumented immigrant, a sexually active 19-year-old whose parents disapprove, a woman in an abusive marriage, a woman who forgot to pack her pills while on vacation … they wouldn't have to. They could walk into a drugstore, consult with a pharmacist, or not, and walk out with a tool to prevent pregnancy.
There's good evidence that OTC contraception could reduce unintended pregnancies. In one 2004 survey, 68 percent of women aged 18 to 44-years-old trying to prevent pregnancy said they would utilize pharmacies for OTC contraceptives such as the pill, the contraceptive patch, the vaginal ring, and emergency contraception. Nearly half of uninsured women and 40 percent of low-income women not currently using any of these methods said they would start doing so if they were available OTC. Studies have also shown that access to multiple pill packs at once results in higher rates of continual use.
OTC birth control pills clearly don't just benefit women—men and society at large gain from fewer unintended pregnancies. Removing health insurance from the contraception equation could lower pill prices. Decreasing unnecessary doctors visits for women could lower health insurance costs and healthcare expenditures overall. It just doesn't make sense from a public health or personal liberty perspective to keep birth control prescription only—though it does make pharmaceutical companies and doctors more money.
"Doctors regularly hold women's birth control prescriptions hostage, forcing them to come in for exams," wrote Stephanie Mencimer in a Mother Jones piece about her own doctor doing so. Dr. Singer described as it doctors extorting pay for a "permission slip" to get the same medication over and over again. Feminist blogger Amanda Marcotte says doctors use "the pill as bait" to make sure women come in once a year.
Both doctors and public health officials publicly worry that women won't receive annual cervical cancer and sexually transmitted infection (STI) screenings without such coercion. How much of this concern is motivated by profit, how much by paternalism, is hard to say.
A 2010 study found 33 percent of doctors always require a pelvic exam and pap smear before prescribing hormonal contraception, and 44 percent regularly do. But there's no medical reason for linking these things. It's like refusing to give someone antibiotics unless they submit to a cholesterol screening.
Perhaps worse, as there's growing evidence that too-frequent Pap smears (which test for cervical cancer) can do more harm than good. The U.S. Preventive Services Task Force now recommends most women only get screened once every three years, not annually. At best, the current overscreening is merely inconvenient and needlessly expensive; at worst, it leads to psychologically-distressing false positives and totally unnecessary but invasive medical procedures.
It's not just some doctors and medical groups who want to keep things status quo. Pharmaceutical companies also gain from it. OTC sales "would drive down the prices substantially," says Singer. Drugmakers can get higher prices from insurance companies than they could in a competitive contraceptive market.
In a 2012 Wall Street Journal op-ed, Louisiana Gov. Bobby Jindal, a self-described "conservative, pro-life" Republican, called OTC birth control a way to "put purchasing power back in the hands of consumers—not employers, not pharmaceutical companies, and not bureaucrats."
Yet the pharmaceutical industry is the only entity with standing to challenge the prescription status of current birth control pills. In order to initiate the switch from prescription to nonprescription, a drug maker must approach the FDA.
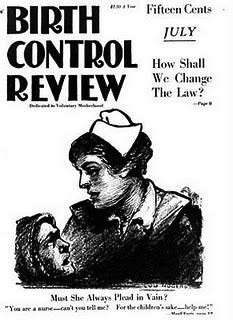
This is pursuant to Section 503(b)(3) of the 1938 Federal Food, Drug, and Cosmetic Act and the 1951 Durham-Humphrey Amendments amendments to it. Testifying about the amendments, Rep. Carl Durham (D-North Carolina) noted that prescription status should be able to be changed when new information came along revealing it no longer necessary for public health protection. That seems to be exactly the situation we've found ourselves in with birth control pills.
"FDA is willing to meet with any sponsor, including those of oral contraceptives, who may want to propose switching their product to OTC status," says FDA spokeswoman Andrea Fischer, which is the same thing the agency has been saying for decades. Unsurprisingly, none of the sponsors who profit from keeping contraceptives Rx-only want to challenge that status.
The New York Times noted that some brand-name birth control pills sell for nearly $100 a month, with insurance companies paying most of it, while generic pills can cost under $10. Drugmakers (and doctors) are benefiting from arbitrarily driving up healthcare costs under a system that doesn't make sense.
That system creates situations like this current Hobby Lobby debacle, where we have the Supreme Court negotiating the thorny space between public interest and religious liberty and progressives arguing in favor of a solution that gives women less reproductive autonomy. "Contraception is a personal matter—the government shouldn't be in the business of banning it or requiring a woman's employer to keep tabs on her use of it," as Jindal wrote in his 2012 op-ed.
OTC birth control could render moot the insertion of employers and Uncle Sam into a woman's birth control decisions. It would reduce the burden on women whose employers won't cover contraception, increase access among the most vulnerable populations, drive down healthcare costs, prevent unintended pregnancies, increase individual liberty (for both contraception users and religious objectors), and bring FDA policy just a small, small step toward being more rational. Yet because of the way America's drug approval process is set up and the incentives pushed by our current healthcare system, it also seems highly unlikely America will see it anytime soon.


Show Comments (41)