American Adults See Occasional LSD Use As Riskier Than Regular Binge Drinking. It's Not.
Fifty years of scaremongering have turned LSD into a bogeyman.
Americans roughly equate the danger of trying LSD once or twice with consuming four to five alcoholic beverages a day, a testament to our country's drug warriors.
Across all age groups, 69.5 percent of respondents "perceive great risk" in trying LSD once or twice, while 68.3 percent of respondents feel similarly about "having four or five drinks nearly every day," according to new survey data released by the Substance Abuse and Mental Health Services Administration. Among respondents over the age of 26: 74 percent saw harm in trying LSD once or twice, while 69 percent saw harm in consuming nearly half a dozen drinks a day.
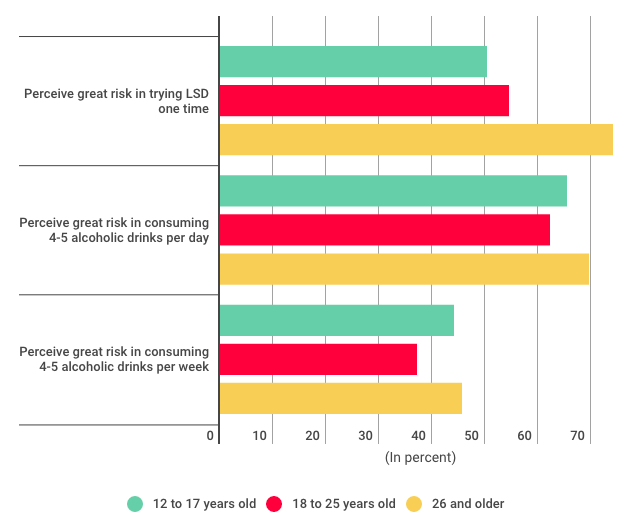
Alas, a majority of American adults are wrong (our youths much less so). Although included in schedule I of the Controlled Substances Act, LSD is a relatively safe, non-habit forming drug, while alcohol is a hepatotoxic sedative that kills roughly 80,000 Americans every year (37,000 of those from liver disease, 9,967 in alcohol-related driving accidents).
In the interest of opening the Overton Window of discourse ever so slightly, let's go through some studies.
In 2010, the British psychopharmacologist David Nutt measured the relative harms of various legal and illegal drugs with a system designed in coordination with other members of Britain's Independent Scientific Committee on Drugs. The committee used 16 criteria to determine a drug's potential harm to the user and to society. The criteria range from easily measurable (drug-specific and drug-related mortality; risk of physical and/or psychological dependence); to nebulous (international damage and community impact). Nutt's team then weighted those factors, combined them into an overall harm score, and, in a paper published in The Lancet, laid the scores out in a very nice chart:
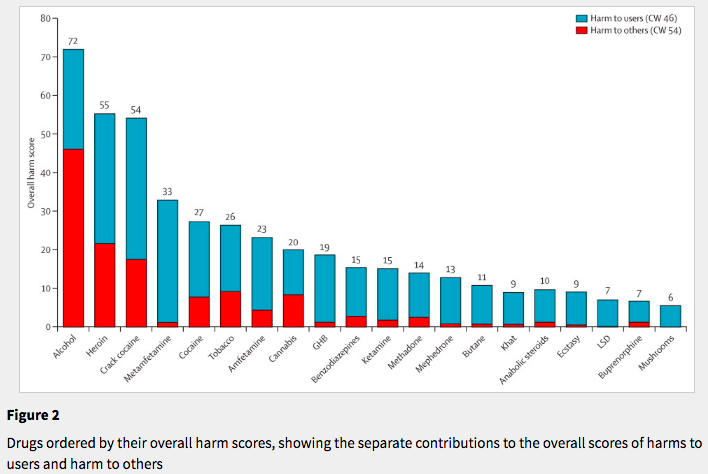
As you can see from the x-axis labels, alcohol is the most harmful drug, followed by heroin. LSD is the third least harmful after buprenorphine (which is common in medication-assisted therapy for opioid use disorder) and psilocybin mushrooms.
The relative safety of LSD has been demonstrated in clinical settings as well. A double-blind randomized control trial to measure the safety of LSD as an adjunct to psychotherapy in 2014 found that "[n]either the experimental dose (200 micrograms of LSD) nor the active placebo (20 micrograms of LSD) produced any drug-related severe adverse events, that is, no panic reaction, no suicidal crisis or psychotic state, and no medical or psychiatric emergencies requiring hospitalization." Two hundred micrograms is twice the dose of the average black market acid tab, while 20 micograms is the amount commonly used by micro-dosing enthusiasts.
What about "acid flashbacks," a concept coined in the 1950s to describe visual distortions that persist or return after psychedelic drugs have cleared the body? A literature review published earlier this year found them to be quite rare:
In addition to a lack of negative acute or enduring mental health effects, no evidence has been found to support the idea that the use of psychedelics leads to any kind of enduring perceptual disturbances, known as 'hallucinogen persisting perceptual disorder' (HPPD) (Krebs and Johansen, 2013b). Despite the high level of vivid mental imagery brought about under the influence of psilocybin, Studerus et al. (2011) found no evidence for enduring visual hallucinations or flashbacks in their pooled analysis of experimental psilocybin recipients. Large-scale population studies have also failed to provide any evidence of HPPD in relation to psychedelic use (Johansen and Krebs, 2015; Krebs and Johansen, 2013b). This is true even in ritual users, who typically have much greater exposure than participants in experimental studies (dos Santos et al., 2016; Halpern et al., 2005).
The 2015 Krebs and Johansen study, published in the Journal of Psychopharmacology, found "no significant associations between lifetime use of psychedelics and increased likelihood of past year serious psychological distress, mental health treatment, suicidal thoughts, suicidal plans and suicide attempt, depression and anxiety."
A 2015 report from SAMSHA on suicide and drug use found that 15 percent of hallucinogen users reported suicidal thoughts; of that group, four percent planned a suicide and two and a half percent made an attempt. While those numbers seem high, SAMSHA and the National Institute of Drug Abuse categorize PCP as a hallucinogen, despite the fact that it is a dissociative anaesthetic and has a very different user demographic than more traditional hallucinogens like LSD, psilocybin, and mescaline. I don't know if the agency's suicide dataset includes reported PCP users, but if it does, their inclusion likely skews the results, as suicidal ideation is a common side effect of long-term PCP use.
The Drug Abuse Warning Network, a project of SAMSHA that tracked drug-related emergency department admissions until its discontinuation in 2011, found a paltry number of LSD admissions in its final year of data collection. DAWN hospitals reported a total of 1.25 million E.D. admissions related to illicit drug use in 2011. Of that number, cocaine was cited in either the chief complaint, the assessment, or the diagnosis in more than 500,000 patient cases, while LSD was cited in only 4,819 cases. An undated DEA fact sheet suggests that LSD E.D. admissions are relatively rare due to the "fewer adverse reactions generated by the low-potency LSD that has been produced since the late 1970's."
As for the positive aspects of LSD: A 2016 analysis of two double-blinded studies conducted in Switzerland found that "LSD positively altered the processing of emotional information by decreasing the recognition of fearful and sad faces and enhancing emotional empathy and prosociality." (Prosociality is a good thing.) Other small trials, some dating back to the 1950s, suggest LSD is a promising treatment for both alcoholism and end-of-life anxiety in terminally ill patients.
And in case you need any more convincing, actor Cary Grant believed LSD saved his life when he tried it in his 50s. "When I broke through, I felt an immeasurably beneficial cleansing of so many needless fears and guilts. I lost all the tension that I'd been crippling myself with. First I thought of all those wasted years. Second, I said, 'Oh my God, the humanity. Please come in.'"


Show Comments (41)