A Phase 3 Clinical Trial Confirms MDMA's Effectiveness As a Psychotherapeutic Catalyst
Subjects diagnosed with severe post-traumatic stress disorder made substantially more progress when they received MDMA rather than a placebo.
MDMA-assisted psychotherapy for people with post-traumatic stress disorder (PTSD) is substantially more effective than psychotherapy alone, according to a study reported today in Nature Medicine. The results of the Phase 3 clinical trial, which are consistent with earlier research, mean that MDMA, which was banned in 1985, is on track to be approved as a prescription drug by the Food and Drug Administration (FDA) as soon as 2023.
"These data indicate that, compared with manualized therapy with inactive placebo, MDMA-assisted therapy is highly efficacious in individuals with severe PTSD, and treatment is safe and well-tolerated, even in those with comorbidities," say University of California, San Francisco, neuroscientist Jennifer Mitchell and her co-authors. "We conclude that MDMA-assisted therapy represents a potential breakthrough treatment that merits expedited clinical evaluation."
The FDA officially recognized MDMA as a "breakthrough therapy" in 2017, meaning it "may demonstrate substantial improvement over existing therapies on one or more clinically significant endpoints." That designation signaled that the FDA would expedite development and approval of MDMA.
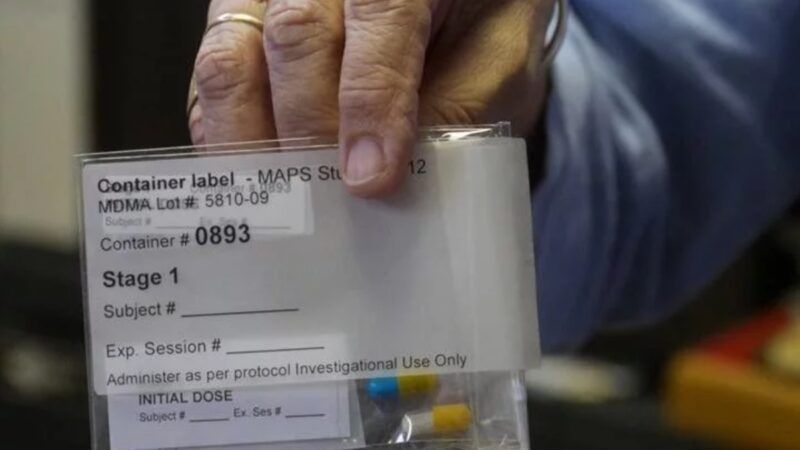
The double-blind, placebo-controlled trial, which was sponsored by the Multidisciplinary Association for Psychedelic Studies (MAPS), confirms MDMA's potential. The study included 90 subjects with "severe" PTSD who were randomly assigned to receive either MDMA or a placebo on three occasions. All of them participated in three preparatory sessions and nine "integrative therapy sessions."
In the MDMA group, scores on the Clinician-Administered PTSD Scale for DSM-5 had fallen by an average of 24.4 points 18 weeks after the study began, compared to 13.9 points in the placebo group. "Functional impairment" based on the Sheehan Disability Scale fell by an average of more than three points in the MDMA group and two points in the placebo group. The subjects who received MDMA also showed bigger improvements in mood as measured by the Beck Depression Inventory II. Their scores dropped by an average of nearly 20 points, compared to about 11 points in the placebo group.
"Three doses of MDMA given in conjunction with manualized therapy over the course of 18 weeks results in a significant and robust attenuation of PTSD symptoms and functional impairment," Mitchell et al. note. "MDMA also significantly mitigated depressive symptoms."
These results are striking but not surprising; psychotherapists have long observed similar effects. As the authors of an earlier MAPS-sponsored study put it, MDMA-assisted therapy is "aimed at allowing participants to revisit traumatic experiences while staying emotionally engaged even during intense feelings of anxiety, pain, or grief without feeling overwhelmed."
Mitchell et al. suggest that "MDMA may exert its therapeutic effects through a well-conserved mechanism of amygdalar serotonergic function that regulates fear-based behaviors and contributes to the maintenance of PTSD." They say MDMA "may facilitate the processing and release of particularly intractable, potentially developmental, fear-related memories," perhaps "by reopening an oxytocin-dependent critical period of neuroplasticity that typically closes after adolescence."
The researchers hypothesize that "the pharmacological properties of MDMA, when combined with therapy, may produce a 'window of tolerance,' in which participants are able to revisit and process traumatic content without becoming overwhelmed or encumbered by hyperarousal and dissociative symptoms." The aim is to "facilitate recall of negative or threatening memories with greater self-compassion and less PTSD-related shame and anger." That process seems to be enhanced by "the acute prosocial and interpersonal effects of MDMA," which "may support the quality of the therapeutic alliance, a potentially important factor relating to PTSD treatment adherence and outcome."
Last year Reason's Nick Gillespie interviewed MAPS founder Rick Doblin, a co-author of the new study. "Although MAPS is doing everything by the book in seeking approval of MDMA as a prescription drug, Doblin's vision goes beyond such doctor-approved uses," Gillespie noted. "He aspires to a world in which people can use psychedelics responsibly without permission from physicians or priests."
Doblin does not accept the idea that psychoactive substances are inherently good or bad. "Psychedelics are tools," he said. "They're not good or bad in and of themselves. It's how they are used. It's the relationship you have with them." He argued that "people should have the fundamental human right to change their consciousness."
