How Will Coronavirus Pandemic Deaths Compare to the 1957 Flu Pandemic?
Social distancing and lockdowns today are why deaths from the two pandemics might be comparable.
How many Americans are going to die of COVID-19? We have been treated to estimates ranging from a catastrophic 2.2 million deaths conjured by an epidemiological model that assumed that people would do nothing in reaction to the pandemic to surmises that the death rate might not be much worse than seasonal flu.
Speaking to CNN's Jake Tapper, National Institute of Allergy and Infectious Diseases Director Dr. Anthony Fauci suggested that between 100,000 and 200,000 deaths could occur. Fauci quickly added that he didn't want to be held to that figure given model imperfections and constantly shifting pandemic trends. Earlier this week, President Donald Trump proffered that keeping the COVID-19 pandemic death rate to between 100,000 and 200,000 would mean that "we altogether have done a very good job."
The White House coronavirus task force is reportedly taking into account the disease and deaths projections made by the University of Washington's Institute for Health Metrics and Evaluation (IHME) model. If current social distancing and stay-at-home requirements are sustained through May, the model estimates that about 84,000 Americans will die of COVID-19 by the beginning of August. The model also forecasts that COVID-19 will peak on April 15 at around 2,214 daily deaths and that June 28 is likely to be the first day where COVID-19 deaths fall below 100 per day.
Interestingly, the number of U.S. COVID-19 deaths projected by the IHME model is similar to those that occurred during the 1957-58 pandemic flu. Researchers estimate that the global case-fatality rate—the percentage of infected patients who died of the disease—was about 0.67 percent for that flu pandemic. That is substantially higher than the typical seasonal flu rate of around 0.1 percent. For the United States, researchers estimate that about 25 percent of Americans were infected by that strain of influenza, killing about 116,000 of them. That would yield a case-fatality rate of 0.27 percent, about three times worse than the seasonal flu average. (A rough calculation assuming a 25 percent infection rate and the same case-fatality rate would project about 223,000 deaths from the current COVID-19 epidemic.)
One of the crucial differences between the 1957-58 flu and the current novel coronavirus epidemic is that no social distancing was implemented as public health policy back in the 1950s. In fact, a special late August 1957 meeting of the Association of State and Territorial Health Officers in Washington, D.C., concluded that, "there is no practical advantage in the closing of schools or the curtailment of public gatherings as it relates to the spread of this disease."
A 2009 article in the journal Biosecurity and Bioterrorism noted that "no efforts were made to quarantine individuals or groups [in 1957-58], and a deliberate decision was made not to cancel or postpone large meetings such as conferences, church gatherings, or athletic events for the purpose of reducing transmission. No attempt was made to limit travel or to otherwise screen travelers." Schools opened as usual and the disease swept across the entire country.
The Biosecurity and Bioterrorism authors concluded that the 1957 outbreak did not appear to have a significant impact on the U.S. economy. They cited a 2006 Congressional Budget Office calculation suggesting that another flu pandemic the size of the one in 1957-58 might reduce real GDP for the year by 1 percent but would likely not result in a recession. In cold-blooded terms, boosting the number of deaths by 100,000 above the annual toll of 1.7 million in 1957 had no deep and lasting effects on the U.S. economy.
As my Reason colleague Jacob Sullum asks, "Is preventing COVID-19 deaths worth a severe recession?" Sullum cogently argues that the answer depends on the lethality of the disease. Unfortunately, the public, politicians, and public health officials won't have a clear answer to that vital question until population screening using serological antibody tests for COVID-19 infections is done.
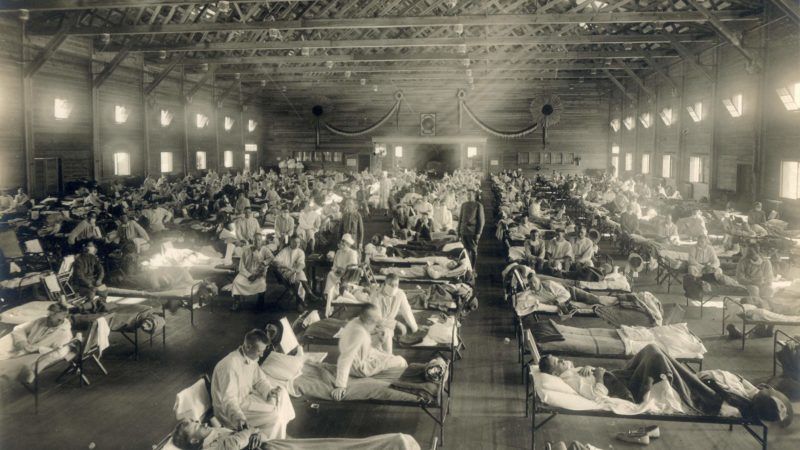
My Reason colleague Brian Doherty cites a brand new study that suggests that early adoption of stringent public health measures, e.g., closing down schools, theaters, churches, and so forth, in response to the 1918 Spanish flu epidemic actually experienced a more robust economic bounce back than cities that reacted more slowly.
In the meantime, assuming that the epidemiological models are even approximately right, the chief reason why the number of COVID-19 deaths in the U.S. may be held down to 1957 pandemic flu levels is because modern public health officials have recommended social distancing measures instead of just letting the current epidemic run its course.

Show Comments (59)