Bad Payments Rise in High Risk Federal Programs
Error-ridden programs paid out $125 billion in improper payments last year.
It's another bad year for bad spending in Washington. The government once again spent more than $100 billion of your hard earned dollars on payments that shouldn't have been made in programs that are known sources of waste and abuse. Indeed, bad payouts
Improper payments, the term of art for this particular form of waste, in 13 federal programs labeled high-risk jumped by $19 billion in the last fiscal year, sources tell Bloomberg Business. According to the report, improper payments in high risk programs came in at $106 billion last year, or 3.5 percent of the total spending in the programs. This year, improper payments are said to come in at $125 billion, or 4 percent of the total. Bad payments, in other words, are growing faster than the programs that are making them.
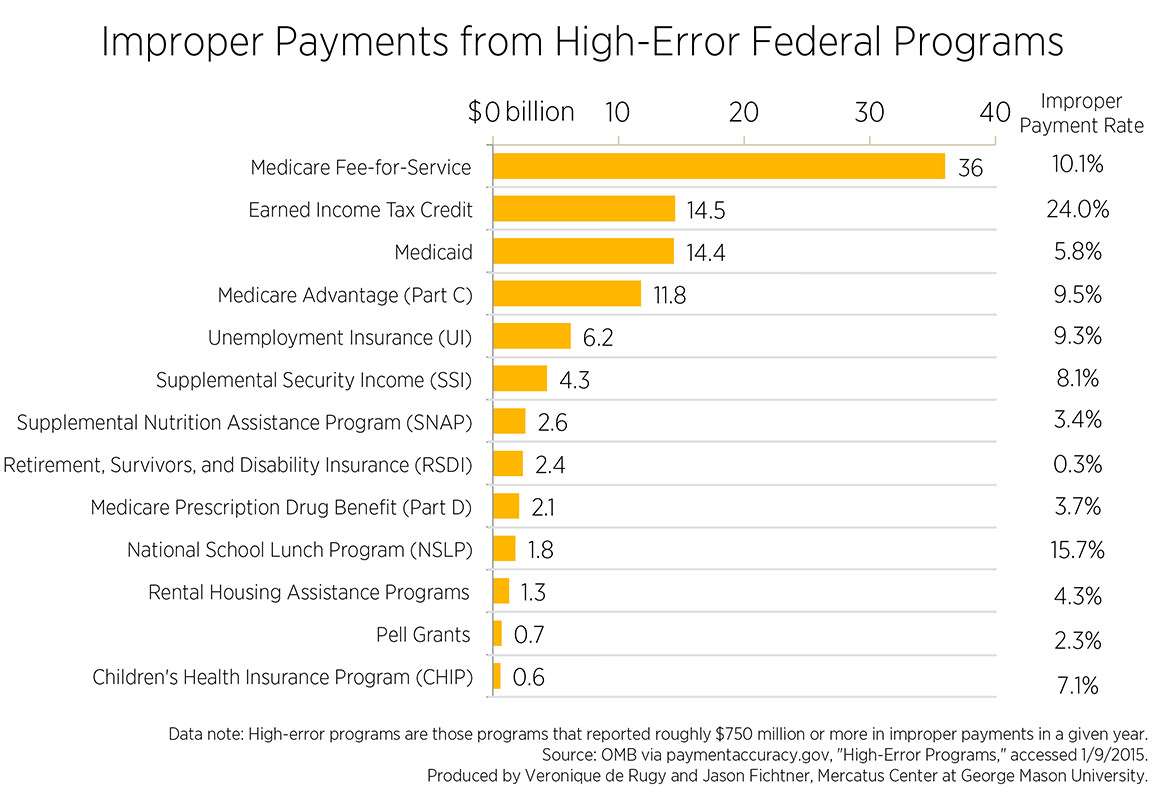
There's no information yet on precisely how the botched spending is divided between programs, but as Bloomberg's report notes, the biggest offenders have previously been health care programs Medicare and Medicaid, as well as the Earned Income Tax Credit (EITC) subsidy for low-income individuals.
As Veronique de Rugy and Jason Fichtner of the Mercatus Center noted last month in a report on payment errors in federal programs, Medicare's improper payment rate was 10.1 percent, while Medicaid's was a comparatively modest 5.8 percent.
Medicare is the biggest spender in dollar terms, which is mostly a reminder of how huge and budget-consuming the nation's single-payer-for-seniors program currently is. But the biggest offender in percentage terms is the EITC, which shells out 24 percent of its total payments improperly. Basically, a quarter of the spending that happens on that program shouldn't have happened or, at a minimum, shouldn't have happened in the way that it did.
You can see the exact amounts and percentages in a chart handily compiled by de Rugy and Fichtner.
None of this is particularly new, of course; these programs are labeled "high risk" because they are serial offenders, blowing billions on bad payments year after year. Medicare was designated by the Government Accountability Office (GAO) as a program at a high risk for fraud back in 1990. Medicaid has been on the watch list since 2003. Every so often, administrators trot out a novel fraud-prevention program, and sometimes there are scattered small scale successes, but for the most part, these programs continue to pay for fraud and abuse year after year, with very little overall improvement. And as the preview of this year's numbers suggests, it's often the case that things get worse, not better.

Show Comments (56)